Functions of the nerve bundle
The tail begins at the level of the 3rd vertebra, located in the lumbar region, and descends below. It is a large bundle of nerve roots emerging from the top of the spinal cord.
Nerve fibers serve to transmit impulses to certain parts of the body and organs, thereby ensuring the vital functions of the human body. The functions of the cauda equina are determined by the large number of nerve roots that form a bundle. This area is responsible for transmitting impulses in the following directions:
- lower limbs;
- pelvic organs;
- sphincter;
- intestines.
Inflammation of this bundle of nerves is accompanied by a number of symptoms. Often the syndrome appears due to compression of the roots located in the lower back.
Clinical picture
Pain appears at the very beginning of the disease. It is concentrated in the lumbar and sacral region, and is remotely felt in the leg on the side of the injury, the groin area. The patient experiences hypersensitivity and poor tactile sensations in terms of painful sensations. When coughing and sneezing, the pain increases significantly, and decreases in a semi-sitting position. A decrease in sensitivity, felt as numbness, indicates increasing hypoesthesia.
Complaints of rapid fatigue while walking and lethargy of the muscles of the lower extremities are signs of motor dysfunction. The more active the pathological process becomes, the more severe the symptoms, and the damage is distributed to the other side of the body. Over time, independent walking becomes difficult.
Disruption of the innervation of the external genitalia leads to a significant decrease in their sensitivity. This, in turn, causes anorgasmia in women and erectile disorders in men. The pelvic organs react with urinary retention and persistent constipation to sensory impairment. Patients are not aware of fullness of the bladder and rectum.
Causes of pathology
Damage, inflammation or compression of the nerve roots leads to disruption of the conduction of impulses to the corresponding organs. This entails impaired organ function, local sensitivity or impaired motor function.
The roots that form the bundle may be damaged or compressed for the following reasons:
- disc herniation;
- lumbar injuries;
- infectious lesions;
- neoplasms in the lower section;
- complication after surgery.
The majority of cases are due to lumbar hernias. A hernia is a protrusion of a deformed disc, which leads to compression of the roots located near the damaged disc. This is accompanied by acute pain, sensory disturbances and other neurological symptoms. The causes of hernia are often degenerative processes in the discs and injuries to the spinal column.
Inflammation of the cauda equina tuft can occur as a result of an epidural abscess of the spine.
Another cause of the syndrome is a congenital malformation of the spine, which results in a narrowing of the spinal canal, which causes compression of the nerve roots.
Often, tail syndrome appears after surgical manipulation of the spine. A factor provoking the development of the syndrome can also be long-term spinal anesthesia.
Cauda equina syndrome. Causes, treatment
Damage or compression of the nerve structures of the cauda equina causes severe pain, weakness of the legs, decreased reflexes, and sometimes loss of sensitivity and paralysis, disorders of the genitourinary system, and intestinal movements. In addition, constant compression of the roots can cause inflammatory processes along the route of the nerve or, for example, require treatment of the sciatic nerve.
In most cases, the disease responds well to conservative treatment of the spine; in extreme cases, when there is a risk of complete immobilization of the patient or the functioning of internal organs is seriously impaired, surgical intervention can be used. But surgery is always considered as a last resort when classical drug treatment fails.
Causes of the disease
The main factors that provoke the occurrence of pain syndrome of the cauda equina may be:
- Traumatic injuries to the nervous structures of the lumbosacral segment of the spinal column (car accidents, falls from a height, fractures of the pelvic or hip bones, vertebral subluxation, bruises or hematomas of the soft tissues surrounding the nerve roots, hemorrhages in the spinal space, complications after surgical operations on the bone structures of the spine or spinal cord, epidural anesthesia, etc.).
- Chronic age-related degenerative-dystrophic changes in the body provoke a decrease in the spinal column, weakening of ligaments, swelling and spasms of muscle structures, as well as compression of nerve fibers (for example, the first symptoms of cauda equina syndrome may indicate the need for treatment for osteochondrosis of the lumbosacral region or osteoporosis). The cause of these diseases lies in a sedentary lifestyle, poor nutrition, bad habits and other factors.
- There is a fairly close connection between the formation of intervertebral hernias in the lumbar region and their compression of the nerve roots. This pattern is observed in 50% of men who came to the clinic with a spinal hernia, and almost all of them were engaged in physically difficult work and noted chronic pain in the back.
- Spinal stenosis is a persistent narrowing of the lumen of the spinal foramen, in which compression occurs not only of the nerve structures of the equine fascicle, but also of the spinal cord itself. It can develop with age-related changes in bone structures - deforming spondyloarthrosis (overgrowth of vertebral osteophytes), displacement of discs forward or backward relative to others - spondylosis, the treatment of which is not given due attention or with congenital anomalies of the spinal column.
Also among the reasons for the progression of cauda equina syndrome are: severe infectious and viral diseases, tumor formations of varying quality, proliferation of metastases, inflammatory processes, complications after spinal puncture, poorly secured metal structures used to treat spinal instability or postural curvature, etc.
Symptoms and diagnosis of cauda equina syndrome
Clinical manifestations of cauda equina syndrome can be quite varied (depending on the location of pathological processes), but over time their intensity and character increase. Pain syndrome from the lower back spreads to the buttocks and along the back of the leg to the lower leg and foot, muscle weakness worsens, sensitivity decreases and muscle reflexes slow down. Disorders of urination and defecation, and potency may be observed.
The starting point for diagnosing the disease is the doctor’s collection of anamnesis of the clinical picture, radiography, and, if necessary, detailed images on MRI or CT equipment. If damage to the spinal cord or neoplasms are detected, it is advisable to additionally undergo a myelographic study. A neurological examination will help identify the patency of nerve impulses and the speed of reflex contractions, and determine the muscle strength of the lower extremities.
After a complete diagnosis, the patient is prescribed conservative drug treatment and, if necessary, surgical intervention. In this case, the operation is intended to eliminate the symptoms of cauda equina syndrome and to prevent the development of chronic paralysis of the legs or disorders of the genitourinary and digestive systems.
Statistics confirm that patients suffering from bilateral nerve damage are much less likely to fully restore limb functionality than those with unilateral pain. Patients with temporary weakening of the pelvic muscle corset have a greater risk of developing paresis or paralysis of the bladder. Therefore, you should not endure pain and at the first signs of the disease you should go to hospitals for treatment of the spine and pinched nerve roots.
Treatment of the disease
Conservative treatment methods. First of all, drug therapy is aimed at relieving pain and reducing compression of nerve fibers. For this purpose, analgesics, non-steroidal anti-inflammatory substances, corticosteroids, and muscle relaxants are used. If necessary, injections of local painkillers (novocaine or lidocaine blockades) may be prescribed. Inflammations caused by persistent infectious or viral processes will require treatment with antibiotics.
The detection of neoplasms or metastases in the spinal cord, bone structures or nearby soft tissues indicates the need for radiation or chemical therapy. Physiotherapeutic procedures (massages, gentle traction of the spine, water procedures, warming, etc.), manual therapy treatment methods (acupuncture, acupuncture, etc.) will help relieve tension and muscle spasms, if possible release the nerve roots, thereby reducing lower back pain and legs.
In the event of a sharp deterioration in the patient's condition and the sensation of the limbs does not recover within 24 hours, immediate surgical intervention is required to avoid complete paralysis of the lower part of the body.
Surgical intervention. Spinal surgery for cauda equina syndrome is usually prescribed on the second day after the cessation of innervation of the limbs or malfunction of the bladder and intestines. At the same time, many doctors claim that the earlier the operation is performed, the faster the lost functions are restored.
Damage or compression of nerve fibers caused by protrusion or herniation of the spine is eliminated by removing part of the vertebral body (laminectomy) or part of the intervertebral cartilaginous disc (discectomy), then neurolysis is performed (careful extraction or release of nerve endings from adhesions or compression by soft structures).
This is followed by a long period of recovery with the use of electrical or magnetic physiotherapy, a gradual return of sensitivity of the limbs, adjustment of the functioning of internal organs, normalization of motor reflexes, and motor abilities are restored much faster than the activity of the pelvic organs.
Author: K.M.N., Academician of the Russian Academy of Medical Sciences M.A. Bobyr
Symptoms of the disease
Symptoms are caused by the functions of the nerve roots of the bundle. Thus, the syndrome is formed by the following disorders:
- pain syndrome in the lower back;
- leg pain;
- weakening of muscles;
- urinary disorders;
- motor impairment;
- malfunctions of the pelvic organs;
- sexual dysfunction in men.
At the beginning of the development of the disease, pain appears. There are two types of pain syndrome - local and radicular. Local pain in the lumbar region has a dull tint, with a tendency to intensify with exercise. Radicular pain is manifested by lumbago, which occurs spontaneously with sudden turns of the body and bending. In this case, sharp pain spreads throughout the affected nerve, so it can be felt in the legs and is accompanied by numbness of certain parts of the body and motor disturbances.
Impaired motor skills in the syndrome are due to the fact that the bundle is formed by motor and sensory nerve fibers. Damage to motor fibers is manifested by gait disturbance, paresis and paralysis of the legs. If sensory fibers are compressed, sensitivity in the groin area and lower extremities is impaired. This is accompanied by a feeling of numbness.
With the syndrome, damage to autonomic fibers is possible, which leads to dysfunction of the skin and hair follicles located on the lower extremities. Patients note a change in the color of their legs, the skin becomes dry and flaky, and hair falls out. In this case, the formation of trophic ulcers on the legs is possible.
From the pelvic organs, most often the syndrome negatively affects the function of the bladder. Symptoms of this disorder include:
- feeling of bladder fullness even after urination;
- rare urge to urinate;
- urinary incontinence.
The disease is often accompanied by impaired intestinal function. Patients complain of constipation, a feeling of bloating and increased flatulence.
Among male patients, sexual dysfunction often develops, including complete impotence.
Diagnostics
A preliminary diagnosis of cauda equina syndrome is made based on the results of a patient examination, medical history, the presence of motor disorders in the lower extremities, impaired sensitivity in the perineal area, decreased reflexes in the lower extremities
Imaging tests include plain x-rays to help identify degenerative changes or injury. MRI (including with contrast) makes it possible to diagnose a tumor, infection, the presence of disc herniations and visualize nerve roots (their degree of compression). Based on the studies, the surgeon can plan the necessary treatment.
But not all people with low back pain and/or leg pain and changes in bowel or bladder function have cauda equina syndrome. Often, bladder problems are associated with a bladder infection (can be diagnosed with a urine test) or diabetes (can be diagnosed with a blood sugar test).
In addition, it is necessary to exclude the possibility of infection or oncological origin of symptoms. Therefore, it is necessary to conduct extensive laboratory tests such as general blood tests, blood biochemistry, serological tests (to rule out syphilis or Lyme disease).
Here is what allows you to reliably diagnose cauda equina syndrome:
- Disease history
- Physical examination: assesses muscle strength, reflexes, sensation, stability and motor abilities.
- Lab tests
- Magnetic resonance imaging (MRI) provides three-dimensional images of the spine.
- Myelogram - an x-ray method of imaging the spine with the introduction of contrast, allowing to determine the pressure on the spinal cord or nerves
- Computed tomography (CT).
Establishing diagnosis
If a person has cauda equina syndrome, consultation with a neurologist is necessary. The diagnosis is made based on examination, testing of reflex activity and diagnostic tests. To exclude organic pathologies, it is necessary to take an X-ray of the spine, as well as an MRI of the lumbar region. This will allow you to assess the condition of the vertebrae and exclude tumors and hernias.
general information
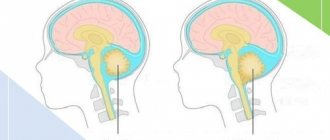
The cauda equina is a bundle of nerve endings located in the lower back. They arise from the terminal part of the spine. They got their name due to their amazing resemblance to a horse's tail. Nerve processes are responsible for the functioning of the large intestine, the normal functioning of the genital organs and the excretory system.
The spinal cord ends in the area of the first lumbar vertebra; the nerves located below (lumbar, sacral and coccygeal segments) are susceptible to various negative factors. Any lesion, regardless of etiology, leads to the appearance of clinical symptoms, movement disorders, and dysfunction of internal organs.
The pathological process is observed mainly in middle-aged patients; women engaged in heavy physical labor are at risk. In children, the disease is rarely diagnosed, with the exception of developmental anomalies of the lower part of the ridge.
Cauda equina syndrome is not a common disease, but it causes serious harm to human health and significantly worsens the quality of life. Treatment in this area is carried out by neurosurgeons and neuropathologists. They should be contacted when the first signs appear for inspection and a comprehensive examination.
Treatment methods
Treatment of pathology largely depends on the cause of the disease. If the cause of the disorder is compression of a bundle of nerves, treatment begins with pain relief. For this purpose, non-steroidal anti-inflammatory drugs are prescribed. For severe pain, corticosteroid injections are indicated. The doctor also prescribes medications to relieve swelling and reduce inflammation, which often accompanies cauda equina syndrome.
For infectious lesions of the spinal cord, treatment with antibiotics is indicated. If the cause of the syndrome is organic pathologies of the spinal cord or spine, treatment of the underlying disease is indicated.
If the pathology is caused by an increase in the size of the hernia, surgical intervention may be necessary.
Causal factors
The main reason for the development of almost any disease of the spine is its congestion, which occurs when lifting heavy objects, prolonged sitting or incorrect posture.
There are a number of reasons that cause compression and damage to the terminal nerve bundle, as well as diseases that lead to the development of the syndrome.
Ossification of the cartilage of the intervertebral disc and loss of its shock-absorbing properties are observed in osteochondrosis. The nerve endings are compressed by a rigid connection and become pinched, which results in pain. If left untreated, degenerative and dystrophic processes in the intervertebral discs lead to their prolapse and the development of a serious complication of the disease - intervertebral hernia, which further compresses the nerve fibers. This pathology is the most common cause of the syndrome.
- Subluxations of the vertebrae, fractures of the sacrum and coccyx are usually accompanied by damage to the nerve trunks. Hematomas formed after injury cause compression. This group of causes also includes iatrogenic injury, which is a complication of epidural anesthesia, neurosurgical operation or spinal diagnostic puncture.
- Benign tumors compress nerve roots, and malignant tumors grow into nerve bundles, causing their destruction. Metastases from malignant tumors of other organs can also provoke the syndrome.
- Congenital narrowing of the lower segments of the spinal column is the cause of compression of the nerve bundles.
- Spondylosis and spondyloarthrosis are acquired deformities of the spine caused by age-related changes in the human body.
- Infectious and inflammatory processes - neuroinfections, osteomyelitis and epidural abscess. The source of infection is chronic foci in the human body: caries, otitis media, tonsillitis, sinusitis, pharyngitis, furunculosis.
- Spondylolisthesis is the slippage of one vertebra from another.
- Demyelination of nerve fibers is a consequence of multiple sclerosis.
- Pathology of the vessels that supply the spinal cord and bleed under some circumstances can cause compression of the nerves.
Damage to the spinal nerves first causes their irritation and hyperexcitability, which is accompanied by pain. Gradually, the function of the nerve trunks weakens. Under the continuous influence of the causative factor, it completely fades away, which leads to motor and sensory disorders in the innervation zone.
Risk factors contributing to the development of pathology:
- Floor. Men are at higher risk of developing the syndrome than women. This is due to faster wear of cartilage and bone tissue.
- Injuries. The occurrence of pathology is facilitated by operations on the spine, injuries, sharp turns and falls on the back.
- Obesity. Fat deposits increase the load on the back, which negatively affects the condition of the intervertebral discs. In obese individuals, muscle tone decreases, and the spine gradually loses its flexibility.
- Smoking. Toxins disrupt the blood supply to the intervertebral discs and increase the risk of developing the disease many times over.
- Passive lifestyle. Office workers, drivers and salespeople are much more likely to develop the syndrome than people in other professions.
- Hereditary predisposition is the presence of diseases of the spine and peripheral nervous system in close relatives.
- Heavy lifting and vibration have a negative impact on the spine.
To study Curvature of the spine in adults, treatment exercises
Surgical treatment
In most cases, it is necessary to decompress the spinal cord nerve bundle using surgical methods. The earlier the operation is performed, the more favorable the future prognosis.
The most unfavorable case is the occurrence of paresis and autonomic disorders in the lower extremities. However, even surgical treatment does not guarantee complete restoration of lost functions.
To restore motor function after surgical treatment, a long course of rehabilitation is required. During this period, treatment is carried out using physiotherapy - electrical stimulation of muscles, massage and manual therapy, therapeutic exercises. The duration of recovery largely depends on the degree of damage to the cauda equina and can last up to six months.
During recovery, sanatorium treatment is recommended.
Signs of the development of the syndrome
The disease can develop and occur with varying intensity and severity of symptoms, depending on the type of roots being compressed, their number and the degree of compression. There are three forms of the disease:
- slowly progressive - the syndrome develops gradually, with mild attacks of sciatica and lower back pain. Over time, the attacks intensify, the intervals between them shorten, and accompanying symptoms appear. The full picture of the disease appears 5-6 months after damage to the nerve fibers;
- acute – the disease occurs suddenly, without previous signs of neurological disorders. The maximum severity of symptoms appears after 3-5 days, the state of health deteriorates sharply;
- intermediate - the severity of symptoms increases gradually, the pain syndrome has periods of remission.
To study Bechterew's disease (ankylosing spondylitis): symptoms, prognosis for life, treatment, tests
The main symptom of cauda syndrome is severe back pain radiating to the buttocks and legs.
Based on the nature of pain, pain is divided into radicular and local. The first type is a sharp shooting pain that covers the area for which the compressed root is responsible. When the body moves, as well as sneezing, coughing, it intensifies and can be felt in the legs, sacral part, perineum, and bladder.
Local pain is dull and deep, it is felt mainly in the spine and adjacent tissues.
In addition to pain, the syndrome has other characteristic symptoms:
- decreased sensitivity - patients experience numbness in the gluteal muscles and thighs, the perineal area, as well as one or both legs from the hips to the feet;
- weakening of the leg muscles - a person has difficulty walking, it is difficult for him to stand, the foot cannot withstand the load. In addition, there are no reflex contractions of the foot and lower leg muscles when acting on the tendons;
- disturbances in the functioning of the bladder and large intestine - constipation, gas, urinary retention or incontinence are noted;
- erectile dysfunction - from periodic disorders to complete impotence, depending on the severity of the lesion.
Treatment of malignant neoplasm of the cauda equina of the spinal cord
Treatment is prescribed only after confirmation of the diagnosis by a medical specialist. Surgical treatment and radiotherapy are used.
Essential drugs
There are contraindications. Specialist consultation is required.
- Etoposide (antitumor agent). Dosage regimen: intravenous drip, for 30-60 minutes. at a dose of 100 mg/m2/day. from 1 to 5 days, repeating cycles every 3-4 weeks.
- Ifosfamide (antitumor drug). Dosage regimen: intravenous drip, for 30 minutes at a dose of 3-5 g/m2 once every 2 weeks.
- Cisplatin (antitumor agent). Dosage regimen: intravenously, as an infusion over 6–8 hours at a dose of 50–100 mg/m2 every 3–4 weeks or 15–20 mg/m2 daily for 5 days every 3–4 weeks.
Possible complications
In the absence of timely comprehensive treatment, cauda equina syndrome can cause serious problems. The patient’s quality of life decreases significantly, and irreversible processes begin. The most common consequences are:
- Inability to move independently, complete loss of motor function.
- Bladder diverticulum, due to overflow and lack of timely emptying.
- Infection of urine as a result of constant stagnation, inflammatory processes in the urethra and kidneys.
- Severe intoxication of the body due to constipation and accumulation of rotting products in the intestines.
Therefore, it is extremely important to consult a doctor when the first signs of illness appear to receive quality medical care. Self-medication or uncontrolled use of traditional medicine recipes can be dangerous to health and life.
Cauda equina syndrome is rarely diagnosed, but the pathology is classified as severe. It requires a comprehensive neurological examination, referral to a computed tomography or MRI, and collection of cerebrospinal fluid for analysis. Detection of the disease is the basis for prescribing comprehensive treatment, which includes medication, physiotherapy and other rehabilitation measures. In some cases, emergency surgical intervention is required to prevent irreversible processes in the body that lead to disability.