Mental illnesses are disorders of brain function. Recognition and treatment of such diseases is the area of interest of psychiatry. But since human mental activity is incredibly complexly organized, it is sometimes very difficult to draw a line that strictly distinguishes the mental norm, its diversity and variability from direct mental deviations. What distinguishes psychiatry from most branches of clinical medicine is that, for the most part, it does not have convincing data regarding the causes, course and outcome of diseases.
- Causes
- Symptoms
- Syndromes of mental illnesses Psychoorganic syndrome
- Seizures
- Blackout
- Catatonic syndromes
- Hebephrenic syndrome
- Hallucinatory-delusional syndromes
- Hypochondriacal syndromes
- Affective syndromes
- Neurotic syndromes
- Dementia
The main criterion for determining the disease is the clinical picture. Although psychiatry became an independent field of medicine more than two centuries ago, and the knowledge of specialists has constantly expanded, the assessment of some mental conditions remains subjective. This is why clinical practice is so important. According to medical literature, certain mental disorders are observed in 2-5% of people. In modern psychiatry, there are several equal classifications of mental illnesses, which are based on different principles. In this article we adhere to the provisions of Russian classical psychiatry.
Causes
Much credible evidence suggests that mental illness arises and develops for many reasons. The main experts believe the following:
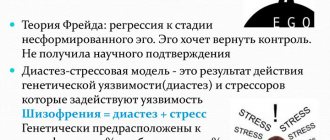
- Heredity. This factor is especially important when it comes to the occurrence of diseases associated with defects in the subtle mechanisms of brain activity, such as the exchange of neurotransmitters, the number and level of development of neuron connections, etc. Scientists have been arguing for a particularly long time regarding the type of inheritance of schizophrenia and epilepsy. According to information from population genetics and genealogical studies, primarily the twin method, we are talking about polygenetic inheritance. Also important in this case is the low penetrance of genes responsible for the inheritance of mental illnesses, which allows them to accumulate contrary to natural selection.
- Biochemical disorders, both caused by heredity and acquired later. Thanks to research in this area, complexes of psychopharmacological drugs have been developed. Most of the hypotheses are divided into three groups to determine the causes of pathology:
- disturbance of neurotransmitter metabolism (the dopamine and neurotransmitter hypotheses determine the role of serotonin, GABA and MAO, which ensure the exchange of mediators);
- disturbance of the metabolism of neuropeptides-endorphins (natural morphinomorphic substances);
- enkephalin metabolism disorder.
- Immunological changes at the level of insufficiency of nonspecific humoral protection, properdin and autoimmune abnormalities. Particularly noteworthy are changes in the activity of T-lymphocytes.
- Mental illnesses of organic nature. They lead to injuries and poisoning. There have been repeated attempts to describe the pathological anatomy of psychoses, but no patterns have been identified at the cellular and macroscopic level.
- Infections, penetration of parasites. A striking example is progressive paralysis, which is a special form of syphilitic damage to the nervous system.
- Psychological traumas leading to changes in “barriers to mental adaptation” and exceeding a person’s compensatory capabilities. The theory has a biological and social basis.
For the most part, psychiatrists divide diseases into two types:
- Endogenous - generated by internal causes (this is schizophrenia, manic-depressive psychosis).
- Exogenous - generated by the environment.
The causes of the second type of disease are more obvious. But, in any case, the pathogenesis of most mental illnesses is only a hypothesis.
Depression
Depression is a common mental disorder and one of the leading causes of disability worldwide. More than 300 million people worldwide suffer from depression. Women are more susceptible to this disorder than men.
Patients with depression are characterized by feeling depressed, loss of interest and the ability to have fun, feelings of guilt, low self-esteem, sleep and appetite disturbances, fatigue and poor concentration. There may even be symptoms that cannot be explained by objective physical causes. Depression, either long-term or episodic, can significantly interfere with daily life, work and school. In the most severe cases, depression can lead to suicide.
Prevention programs exist to help reduce the incidence of depression in both children (for example, by providing protection and psychological support after physical or sexual abuse) and adults (for example, by providing psychological support after natural disasters and conflicts).
There are effective treatments. Mild to moderate depression can be treated with narrative therapy, particularly cognitive behavioral therapy and psychotherapy. Antidepressants have been used successfully to treat moderate to severe depression, but are not the first choice for mild depression. They are not used to treat depression in children and are used with caution and not primarily in the treatment of depression in adolescents.
Management of patients with depression should include psychosocial elements, particularly identifying stressors such as financial problems, work difficulties or psychological abuse, and sources of support such as family and friends. It is important to ensure that social interaction and participation in society are maintained and renewed.
Symptoms
Symptoms and syndromes of mental illness are described by general psychopathology. They are very diverse; many classifications have been adopted that take into account areas of mental activity to which it is possible, although somewhat conditionally, to apply symptoms (emotional, thinking, volitional disorders, as well as memory and perception disorders). But the authors of all classifications especially pay attention to the ambiguity of the manifestations of the disease. The following are the main groups of symptoms, their definition and necessary explanations. In some cases, literary examples will be given to illustrate dry definitions.
Receptor disorders are the most elementary signs of mental illness, to which experts include the following disorders:
- hyperesthesia is increased sensitivity to external stimuli that are neutrally perceived by people in a normal state. For example, the light seems too bright, sounds are incredibly loud, touches are harsh. Moreover, in reality, the strength of the stimulus does not go beyond the threshold familiar to the body;
- hypoesthesia - decreased sensitivity when objects appear shapeless, dull, and without intonation;
- senestopathy - vague painful feelings that come from parts of the body - “burning”, “itching”, “pulling”, “pressing”, although there is no reason for them;
- metamorphopsia - incorrect perception of the size and shape of phenomena in the surrounding world: the illusion of curvature of the space of a room, the apparent lengthening of a street or body;
- Derealization is a very complex symptom when the patient feels the illusory nature of the material world. Objects are seen as in a dream, the sense of reality is lost, there is practically no distinction between “previously seen” and “never seen”, well-known things seem unknown and vice versa;
- personified awareness - the patient, being in an empty room, simultaneously feels someone’s presence and is aware of his loneliness;
- violation of awareness of time - it “moves” sometimes quickly, sometimes slowly, sometimes “it’s not there”;
- Apperception disorder – the patient cannot establish a connection between phenomena or understand the meaning of the phenomenon.
Disorders of the ability to navigate (in time, in a situation, in an area, in one’s personality):
- confusion is a painful state of mind, perceived as extraordinary, attempts to find out: “What was that? What's happened?";
- Depersonalization is a violation of awareness of one’s personality, a person feels his own thoughts, feelings, actions as alien, introduced, and loses self-awareness.
Feeling disorders are a whole group of symptoms, some of them can occur in a healthy person as a result of the influence of certain factors. Among them are:
- hyperthymia is an overly cheerful mood in which drives intensify, vigorous activity develops, a person believes himself to be free from absolutely all diseases, and is optimistic about the future. Extreme degree of severity – euphoria, ecstasy;
- hypothymia (depression) – despondency, sadness;
- dysphoria - a person is overcome by gloominess, gloominess, anger, he becomes aggressive;
- fear – extreme tension that arises in anticipation of a certain threat;
- anxiety - a feeling of threat from nowhere;
- lability – the patient’s mood changes without any reason;
- apathy - complete indifference to oneself and what is happening around;
- a feeling of loss of feelings - an extremely strong emptiness of emotions experienced by the patient, when “both joy and sadness have disappeared.”
Thought disorders have a variety of symptoms, some of which are evidence of very serious mental disorders. Among these signs:
- acceleration of thinking - a person too easily generates thoughts, associations, images, and there is a tendency to be distracted. The extreme manifestation of the symptom is mentism - a flow of thoughts that cannot be controlled;
- inhibition of thinking - in the case when new associations and images arise with difficulty, because they are interfered with by existing ones - this is thoroughness of thinking. But when there is only one thought for a long time, and a person expresses it automatically in all situations, perseveration of thinking is diagnosed;
- incoherent thinking - the patient loses the ability to establish associative connections, cannot carry out basic generalizations, analysis or synthesis;
- blockage of thinking - an unmotivated stop in the thinking process, thoughts and speech are cut off;
- paralogical thinking is a combination of ideas and images that cannot be compared.
Obsessions, also called compulsions:
- abstract obsessions (counting, mental reproduction of events and images);
- sensory obsessions (persistent unpleasant thoughts);
- an ongoing feeling of disgust;
- blasphemous thoughts;
- mastering ideas - a person takes the fictitious for the real, contrary to logical reasoning;
- obsessive urges - the patient has a desire to perform this or that action, it is impossible to resist this impulse;
- Phobias are obsessive, unfounded fears. Today, almost 400 species have been described;
- obsessive doubts;
- obsessive actions - some of them are a protective ritual that protects against phobias, some arise on their own. But at the same time, they are not all uncontrollable.
Delusion is an irreparable establishment of a connection between phenomena and incidents, devoid of any valid basis. It is accompanied by a conviction that cannot be shaken, although illogicality and lack of motivated connections (crooked logic) are visible to the naked eye. Delirium completely takes over consciousness. There is a primary (interpretative) delusion, which is formed on the basis of real facts and incidents that have been processed, distorted and supported by a certain number of false or unmotivated arguments.
The second type of delusion is sensory (figurative), which necessarily occurs in combination with other disorders. It is evidence of an acute condition. Such nonsense lacks a system, it is fragmented and inconsistent. As a result of treatment, figurative delusions may remain the only symptom. In this case, it is called residual. In some cases, induced delusions occur in people who have been forced to be in contact with a mentally ill person for a long time. It reflects the theme of the patient's delirium, but quickly disappears after contact is stopped. It is necessary to distinguish from delirium overvalued ideas that arise as a result of certain circumstances, but occupy too significant a place in the consciousness.
- Perception disorders - they are false ideas that arise involuntarily in the area of one or more analyzers:
- Hallucinations are perceptions that occur when there is no real stimulus. They are presented as visions, sounds, smells, sensations (warmth, cold). In reality, none of the above exists, although the patient does not doubt their reality;
- pseudohallucinations - are perceived as “special” images that actually exist, which the patient perceives as the result of the action of an outside will, for example, a visible image behind one’s back, voices in the head;
- hypnagogic hallucinations - visions that appear in a dark field of vision immediately before falling asleep;
- hypnopompic hallucinations - appear at the moment of awakening;
- illusions are distorted perceptions of existing objects and phenomena, characterized by the fact that the image of a real object is combined with the presented one;
- functional hallucinations - appear only when a real external stimulus is present, existing in parallel with it, without being combined until the end of the impact. This could be a reaction to the sound of water, the sound of wheels, music, the howling of the wind, etc.;
- reflex hallucinations - occur in the sphere of another analyzer, and not in the one directly affected by the stimulus.
Memory disorders . Memory gives us the opportunity to record information “in our head” and reproduce it at the right moments. When a person has a memory disorder, he may experience the following conditions:
- fixation amnesia
- amnesia
- cryptomnesia
- confabulation
- progressive amnesia
Amnesia refers to a state where a person “erases from memory” certain events or the entire past without his own decision. With a fixation type of amnesia, the patient cannot remember what is happening to him at the current time. With a progressive type of amnesia, the patient first forgets what happened recently, and gradually begins to forget more and more ancient events. The term "confabulation" refers to false memories. That is, a person allegedly remembers events that never happened to him.
Impulse disorders . This is an increase or, conversely, a decrease in the dynamic properties of the individual. A person may be inappropriately active or passive, too proactive or with no initiative at all. Basic impulse disorders:
- hyperbulia
- abulia
- raptus
- stupor
- akinesia
- hyperbulia
A mental illness in which a person has increased willpower, active impulses and the desire to realize desires is called hyperbulia. Akinesia means the absence of voluntary movements, which causes a person to become immobile. The opposite condition is called raptus. A person with this disorder has frantic motor agitation, and such patients can be aggressive.
Desire disorders. This group includes well-known disorders: anorexia and bulimia. Polydipsia is also included here; This is a condition in which a person constantly wants to drink. Among desire disorders there are also more complex diseases associated with sexual desire.
Impulsive actions and attraction. People with such mental illnesses do things unconsciously, without motivation. From the outside, the action can be described as ridiculous. Aggression may be present. This includes dipsomania, pyromania, and kleptomania. The last of these disorders is widely known. It is characterized by the desire to appropriate other people's things, even those that do not carry any value.
Speech disorders. The symptoms of this group are recorded mainly in neurological disorders. Mental disorders include those related to speech:
- schizophasia
- paralogy
- intermittent speech
- symbolic speech
- incoherence
- echolalia
- verbigeration
- cryptolalia, etc.
Syndromes of mental illness
Mental illnesses consist of certain syndromes. Syndromes are sets of symptoms that are important for diagnosing a disease. By changing syndromes, a doctor can recognize one or another mental disorder. Syndromes must be accurately identified to treat and prognose the disease.
Psychoorganic syndrome
It is a consequence of organic damage to the brain, which occurs with brain tumors, intoxication, atherosclerosis of cerebral vessels and injury to this organ. The syndrome includes:
- weakening of understanding
- memory impairment
- affect incontinence
- affective lability
There may be small delusional ideas that are aimed at those closest to you. A person may think that he is constantly being watched, that a certain thing has been stolen from him, etc. In some cases, such patients experience hallucinations, mainly auditory. Neurological symptoms are present in 100% of cases.
Seizures
These are sudden, short-lived conditions in which a person loses consciousness and makes convulsive movements (or other involuntary movements). Seizures can be different. Grand mal seizure is common. Before it, a person begins to have a headache, he becomes lethargic, and has difficulty working. This state lasts from 2 to 4 hours. Then hallucinations arise, a state of derealization occurs. A person perceives the shape of the objects he sees differently. Autonomic disorders lasting 2-4 seconds are typical. Then the person faints, and a tonic contraction of the body muscles begins. He falls to the ground, screaming loudly. Then the so-called tonic convulsions begin, followed by clonic convulsions, during which foam flows from the mouth. After this, the person falls into a comatose state and then falls asleep. After 2-4 hours the patient returns to consciousness. He doesn’t remember about the convulsions and coma and can’t talk about it.
Blackout
A person either does not completely perceive reality, or perceives everything around him very vaguely; loss of orientation occurs, thinking is disrupted, and the person does not remember events well. In case of clouding of consciousness, urgent assistance from a doctor is needed. These conditions include:
- delirium
- stun
- amentia
- oneiroid, etc.
In the last of these conditions, a person sees scenes that do not exist in reality, and silently watches them, without trying to take part or escape. He remembers everything that happened.
With twilight clouding of consciousness, a person can commit actions that pose a threat to others. After the patient returns to normal consciousness, he characterizes what was committed as alien actions. There are also fugues. These are conditions in which a person performs stereotypical actions, and when consciousness returns, he does not remember what happened.
Catatonic syndromes
It can be like excitement, in which a person is absent-minded, mannered, his speech is not connected, his thinking is impaired, there are impulsive movements. And the second form of catatonic syndromes is completely opposite, it is called catatonic stupor. The person is flexible, like wax, or his muscles become numb.
Hebephrenic syndrome
The condition of patients with this syndrome is characterized by speech and motor agitation. Behavior is characterized as mannered and foolish, and ridiculous actions are possible. Cheerfulness is not caused by external reasons. Often patients with this syndrome commit antisocial actions. In this case, thinking is characterized as fragmented; there may be delusional states and fragmentary hallucinations. Catatonic symptoms are possible in some cases.
Hallucinatory-delusional syndromes
A person experiences a large number of hallucinations in which consciousness remains clear. Paranoid syndrome is typical, which in some cases has an acute beginning and end, etc. This also includes paraphrenic syndrome, which is characterized by fantastic delusions of grandeur, systematized delusions of persecution, etc.
Hypochondriacal syndromes
A person with such mental illnesses places excessive emphasis on health. He constantly has a fear of getting sick (and the fear may be of a certain pathology). Patients complain about their health, may constantly make appointments with a doctor, and hypochondriacal delirium is likely. Hypochondriacal syndromes are also characterized by delusions of physical impairment. That is, the patient begins to believe that there is something wrong with his appearance, and he needs to have surgery as soon as possible to eliminate this defect.
Affective syndromes
This includes the well-known manic syndrome. People with this diagnosis have accelerated thinking, typical hyperthymia, and are very active. This group of diseases also includes depressive syndrome, in which thinking slows down, movements become slow and smooth, and hypothymia is characteristic.
Neurotic syndromes
This group includes:
- hysterical states
- asthenic syndrome
- phobias
A classic hysterical attack is extremely rare today. A person in a seizure falls to the floor (without hitting anything) and makes expressive involuntary movements (very different from seizures). In some cases, the body resembles an arc, since the patient rests on the ground/floor with his heels/feet and the back of his head. The pupils react to light normally.
Dementia
This is an impoverishment of mental activity that is irreversible. Moreover, the disease can be either congenital or acquired. The last form is called dementia. It can be caused by poisoning of the central nervous system with medications or other substances, severe brain injury, or encephalitis. Some of the patient's cognitive functions may be reduced. The person has impaired attention, memory, etc.
Classification of mental illnesses
In classical psychiatry the following classification is accepted:
- endogenous mental illnesses
- endogenous-organic
- exogenous-organic
- exogenous
- psychogenic
- pathology of mental development
The last of the listed groups includes psychopathy and mental retardation (dementia, which is found in a person from birth). Psychogenic diseases are reactive psychoses and neuroses. Smoking and alcoholism, as well as symptomatic psychoses, are classified as exogenous mental disorders.
Schizophrenia and other psychoses
Schizophrenia is a severe mental disorder that affects 21 million people worldwide. Psychoses such as schizophrenia are characterized by distorted thinking, perception of the world and self, emotions, speech and behavior. Common psychotic symptoms include hallucinations (hearing, seeing, or feeling things that are not there) and delusions (persistent false beliefs or suspicions that persist even in the face of evidence to the contrary). People with these disorders may have difficulty working and learning.
Lack of access to health and social services can result in stigma and discrimination. In addition, people suffering from psychosis are at high risk of human rights violations, for example, during long-term institutionalization.
Schizophrenia typically develops in late adolescence or early adulthood. There are effective drug treatments combined with psychosocial support. With proper treatment and social support, patients can lead productive lives and integrate into society. Assistance and care in activities of daily living, housing and employment support can provide the foundation from which people with severe mental disorders, including schizophrenia, can achieve multiple recovery goals, as they often have difficulty obtaining or maintaining a regular job or housing.