These paths can be divided into two groups:
1) the main motor, or pyramidal, pathway, tractus pyramidalis (cortical-nuclear and corticospinal tracts), carries impulses of voluntary movements from the cerebral cortex to the skeletal muscles of the head, neck, trunk, and limbs through the corresponding motor nuclei of the brain and spinal cord;
2) extrapyramidal motor pathways, tractus rubrospindlis, tractus ves-tibulospinalis, etc., transmit impulses from the subcortical centers to the motor nuclei of the cranial and spinal nerves, and then to the muscles.
Pyramid Path
tractus pyramidalis , refers to a system of fibers along which motor impulses from the cerebral cortex, from the precentral gyrus, from giant pyramidal neurons are sent to the motor nuclei of the cranial nerves and the anterior horns of the spinal cord, and from them to the skeletal muscles.
The pyramid path is divided into three parts:
1) corticonuclear - to the nuclei of the cranial nerves;
2) lateral corticospinal (pyramidal) - to the nuclei of the anterior horns of the spinal cord;
3) anterior corticospinal (pyramidal) - also to the anterior horns of the spinal cord.
Corticonuclear pathway
tractus corticonuclearis, is a bundle of processes of giant pyramidal neurons, which from the cortex of the lower third of the precentral gyrus descend to the internal capsule and pass through its knee. Next, the fibers of the cortical-nuclear tract go to the base of the cerebral peduncle, forming the medial part of the pyramidal tracts. The corticospinal and corticonuclear tracts occupy the middle bases of the cerebral peduncle. Starting from the midbrain and further, in the pons and medulla oblongata, the fibers of the corticonuclear tract pass to the opposite side to the motor nuclei of the cranial nerves: III and IV - in the midbrain; V, VI, VII - in the bridge; IX, X, XI, XII—in the medulla oblongata. In these nuclei, the cortical-nuclear (pyramidal) pathway ends; its constituent fibers form synapses with the motor cells of these nuclei.
Central and peripheral paralysis, localization of the lesion, clinical manifestations.
Page 1 of 13Next ⇒
Cortico-muscular tract, localization of central and peripheral neurons in the cortex, brain stem, spinal cord.
The cortico-muscular tract is a two-neuron pathway that connects the cerebral cortex with the skeletal (striated) muscles.
The pyramidal system is the collection of all central motor neurons.
This pathway consists of two neurons: the central (upper) motor neuron; peripheral (lower) motor neuron.
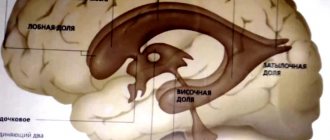
The central neuron is located in the area of the following gyri: the upper part of the precentral gyrus (movement of the lower limb); middle section of the precentral gyrus (upper limb movement); the lower part of the precentral gyrus (movements of the head, face, tongue, pharynx, larynx); posterior section of the superior frontal gyrus (trunk movements); posterior section of the middle frontal gyrus (rotation of the head and eyes in the opposite direction); Neurons are located mainly in the 4th cytoarchitectonic field (according to Brodmann), as well as in neighboring fields. The central neuron originates from the large pyramidal cells of Betz, located in the fifth cortical layer.
The impulses of pyramidal cells follow two paths: cortical-nuclear (ending in the nuclei of the cranial nerves); corticospinal (ends in the anterior horn of the spinal cord). The axons of all these nerve cells go down and inward, forming a corona radiata in the white matter. Then they pass into the internal capsule ( corticonuclear tract - knee of the internal capsule; corticospinal tract - anterior two-thirds of the posterior thigh of the internal capsule). After leaving the internal capsule, both bundles pass into the cerebral peduncles ( the corticonuclear tract is located medially, the corticospinal tract is located laterally ). In the pons, the tract passes at the base and is divided into separate bundles. Within the brain stem, one part of the corticonuclear fibers passes to the opposite side, providing bilateral innervation for the oculomotor, masticatory muscles, for the upper facial muscles, for the muscles of the pharynx and larynx. The other part of the corticonuclear fibers passes completely to the opposite side; the muscles of the lower half of the face and the muscles of the tongue receive innervation only from the cortex of the opposite hemisphere. The central neurons of the cortical-nuclear pathway form synapses with peripheral neurons in the nuclei of the cranial nerves: (trigeminal, facial, glossopharyngeal, vagus, hypoglossal). The axons of peripheral neurons of the corticonuclear tract constitute the motor fibers of the cranial nerves. The fibers of the corticospinal tract come together and form two ridges on the surface of the medulla oblongata - pyramids . 80-85% of the fibers of the corticospinal tract, at the border of the medulla oblongata and the spinal cord, pass to the opposite side and form the lateral pyramidal fasciculus , the rest of the fibers descend uncrossed in the anterior cords of the SM - the anterior pyramidal tract. Uncrossed fibers cross at the segmental level through the anterior commissure of the SC. In the cervical and thoracic parts of the SC, some fibers connect to the anterior horn cells of their side, so that the muscles of the neck and trunk receive cortical innervation on both sides.
The cells of peripheral neurons of the corticospinal tract are located in the anterior horns of the SC and their axons are part of the anterior motor roots and constitute the motor fibers of the peripheral spinal nerves.
Central and peripheral paralysis, localization of the lesion, clinical manifestations.
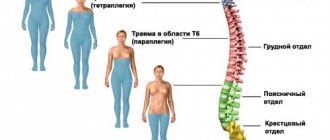
Paralysis and paresis are the loss or limitation of motor function, characterized by the absence (paralysis) or decrease (paresis) of muscle strength, as a result of which the performance of movements is impossible or difficult. Depending on the location and extent of the lesion, movement disorders may be observed: monoplegia; paraplegia; hemiplegia; diplegia; triplegia; tetraplegia.
Central paralysis occurs when central motor neurons are damaged at any level of the corticospinal tract.
Symptoms of central paralysis:
- decreased strength combined with loss of fine movements; — hypertonicity (spastic increase in tone); - increased proprioceptive reflexes with or without clonus; - reduction or loss of exteroceptive reflexes (abdominal, cremasteric, plantar); - the appearance of pathological reflexes; - protective reflexes; — pathological conjugal movements (syncinesia); - absence of degeneration reaction.
Spastic paralysis – increased muscle tone. Clonus is an extreme degree of increase in deep reflexes and expansion of their reflex zone.
Pathological reflexes: On the lower limb, pathological reflexes are divided into extension and flexion.
Extensor: Babinski reflex - in response to line irritation of the foot - extension of the first toe, fan-shaped divergence of all the others; ref-s of Oppenheim - extension of the first toe in response to pressing the pad of the first finger of the hand along the anterior surface of the shin; Gordon's ref - extension of the first finger or the entire lower limb when the calf muscle is compressed by the hand; ref-s Shevera - extension of the thumb in response to compression of the heel tendon; ref-s Cheddon - extension of the first foot with line irritation of the skin of the ankle in the direction from the heel to the back of the foot; ref-s of Grossman - extension of the Ip foot with compression of the distal phalanx of the V p foot.
Flexion: ref Rossolimo - with abrupt blows to the distal phalanges of the fingers, rapid plantar flexion of all toes occurs; ref-s Bekhterev-Mendel - when tapping on the dorsum of the foot in the region of the 3-4 metatarsal bones - rapid flexion of 2-5 fingers; ref-s of Zhukovsky-Kornilov - plantar flexion of the II-IV foot when hitting the plantar side of the foot closer to the toes; upper ref-s Rossolimo - flexion of the distal phalanx of the hand with a short blow to the tips of 2-5 fingers; ref-s Rossolimo-Venderovich - the blow is applied to the distal phalanges of slightly bent 4-5p; ref-s Bekhterev - nodding movement 2-5p when hitting the back of the hand in the region of 2-4 metacarpal bones; ref-s Zhukovsky - flexion 2-5p in response to a blow to the palmar surface of the hand in the region of the 3-4 metacarpal bones; Hoffmann's ref. - bending movement of the fingers in response to pinch irritation of the nail plate of the 3rd point of the hanging hand; ref-s Klippel-Weil – flexion of 1 hand with passive extension 2-5p; Jacobson-Lask sign – palmar flexion of the fingers when the lat part of the carpal-radial joint is struck.
Pathological reflexes carried out by the oral muscles : nasolabial reflex - when tapping on the back of the nose, contraction of the orbicularis oris muscle (pulling the lips forward); proboscis reflex - when tapping on the upper/lower lip, the lips are pulled forward.
Protective reflexes : ref. Bekhtereva-Marie-Fois - with increased passive plantar flexion of the fingers or foot, flexion occurs in the hip, knee and ankle joints; ref-s Remaka - with line irritation of the skin of the upper third of the anterior thigh, plantar flexion of the foot, 1-3 toes and extension of the lower limb at the knee joint occur; shortening ref-s Davidenkova - when irritating the foot of a paralyzed limb or attempting to plantar flex the foot, flexion occurs in the hip and knee joints and extension in the ankle.
Synkinesis is a reflex friendly movement of a limb (or other part of the body), accompanying the voluntary movement of another limb (part of the body). If the patient, according to the instructions, resists with his healthy hand the extension in the elbow joint produced by the examiner, or strongly shakes his hand with his healthy hand, then a concomitant reflex flexion occurs in the paralyzed arm.
Peripheral paralysis occurs when the second neuron of the two-neuron motor pathway, which takes part in the innervation of the muscle, is damaged, i.e. cells of the anterior horns of the SC, anterior roots and motor fibers of the spinal and cranial peripheral nerves. Har-sya: loss of reflexes; muscle atony or hypotonia; muscle atrophy; reaction of rebirth. The degeneration reaction is a change in the electrical response of the affected nerves and muscles, characteristic of peripheral paralysis. During the degeneration reaction, the nerve does not conduct current to the muscle because the nerve is damaged, the muscle itself is denervated and is not able to contract when it is directly irritated by current. With peripheral paralysis, fibrillar twitching can be observed in atrophic muscles - rapid contractions of individual muscle fibers or their bundles.
| Damage level | Symptoms |
| Precentral gyrus of the frontal lobe: A) focus of destruction B) focus of excitation | A) contralateral central or spastic monoparesis. B) epileptic seizures (focal, tonic, tonic-clonic, clonic motor seizures). |
| Inner capsule | Controll spastic paralysis, hemianesthesia, hemianopsia, hemiplegia, center paresis 7, 12 par. |
| Trunk, damage to peripheral motor neurons and motor neuron cables (fibrillation/fasciculation). | Flaccid backplate paralysis of the muscles innervated by these nuclei. Intermittent (alternating) syndrome, the sides where the lesion is observed alternate (3 floors). Weber's syndrome - when the cerebral peduncle is damaged on the side of the lesion, there is damage to the oculomotor nerve, and on the opposite side - spastic hemiplegia or hemiparesis. Jackson syndrome is a syndrome of peripheral paralysis of the muscles of half the tongue on the side of the pathological lesion in combination with hemiparesis or hemiplegia of the central type on the opposite part. Millard-Gubler syndrome is a peripheral paralysis of the facial muscles on the side of the lesion and hemiplegia on the opposite side. |
| Upper cervical segment C1 – C4 | Central tetraparesis (plegia), paresis of the diaphragm, disturbance of the autonomic functions of the pelvic organs according to the central type, loss of all types of sense below paralysis from the level of the back of the head. |
| Cervical thickening C5 – Th2: A) anterior horns B) lateral columns | A) combined tetraplegia: combined upper flaccid paraplegia, lower spastic paraplegia B) combined: left-sided upper flaccid monoparesis, conduction-type decreased senses, left-sided lower spastic monoparesis, impaired pelvic organs. Horner's syndrome: miosis, ptosis, enophthalmos. Violation of the sympathetic innervation of the pupil - (in the lateral horns - ciliospinal center C8 - Th2). |
| Upper thoracic region | Immobile chest, flaccid paralysis of the external intercostal muscles, central paralysis of the lower extremities (spastic paraparesis), disorder of the pelvic organs according to the conduction type. |
| Lower thoracic region Th7 – Th12 | Central paralysis of the lower extremities (paraplegia), disturbance of the pelvic organs according to the central type, conduction disturbance of the senses. |
| Lumbar thickening (in the anterior horns) | Lower flaccid paraparesis, disturbance of the function of the pelvic organs according to the central type, conduction disturbance of the senses. |
| Epiconus L4–S2 | Prolapse, flaccid paralysis of the muscles of the posterior thigh, lower leg, buttocks on the affected side. |
| Cone S3 – S5 | Loss of sensation in the perineal region, true incontinence, peripheral dysfunction of the pelvic organs. |
| Ponytail | Pain! Sluggish asymmetric paresis of the lower extremities, disturbances of the pelvic organs of the peripheral type. |
| Spinal cord: A) anterior horns B) anterior roots | A) fibrillary twitching B) fascicular twitching |
| Peripheral nerve | Flaccid paralysis, paresis. |
1Next ⇒
Recommended pages:
Use the site search:
Lateral and anterior corticospinal (pyramidal) tracts
tractus corticospinales ( pyramidles ) lateralis et ventralis , also begin from the giant pyramidal neurons of the precentral gyrus. The axons of these cells are directed to the internal capsule, pass through the anterior part of its posterior peduncle, and descend to the base of the cerebral peduncle. Next, the corticospinal fibers descend into the anterior part (base) of the pons and exit into the medulla oblongata, where they form pyramids. In the lower part of the medulla oblongata, part of the fibers passes to the opposite side and continues into the lateral cord of the spinal cord. This part of the pyramidal tracts, involved in the formation of the pyramidal decussation (motor decussation), is called the lateral corticospinal (pyramidal) tract. Those fibers of the corticospinal tract that do not participate in the formation of the pyramidal decussation and do not pass to the opposite side continue their journey down as part of the anterior cord of the spinal cord. These fibers make up the anterior corticospinal (pyramidal) tract. Then these fibers also pass to the opposite side, but through the white commissure of the spinal cord and end on the motor cells of the anterior horn of the opposite side of the spinal cord.
Corticospinal (pyramidal) and corticonuclear tracts
carry out conscious voluntary regulation of movements. These pathways are made up of a chain of two neurons - the central
and
peripheral.
Central neurons are
the cells of the cortical nucleus of the motor analyzer,
which end in the motor nuclei of the cranial nerves (fibrae corticonuclearis) and in the motor nuclei of the anterior horns of the spinal cord
(tractus corticospinalis).
Peripheral neurons are
cells of the motor nuclei of the cranial nerves
and
the motor nuclei of the spinal cord,
the processes of which, as part of the nerve trunks, end in the corresponding muscles with motor endings. The pyramidal tract conducts impulses from the cortical nucleus to the active part of the motor system - the muscles. These impulses arise in the cortex as a result of the analysis and synthesis of stimuli received through the proprioceptive pathway, as well as through other pathways (visual, vestibular, auditory, cutaneous). The bulk of the fibers are made up of axons of pyramidal cells of the precentral gyrus.
In the middle sections of the pons, a bundle of fibers is separated from the motor pathway to the motor nucleus of the trigeminal nerve of its own and opposite sides. From the cells of these nuclei, motor fibers of the trigeminal nerve arise, which, as part of the mandibular nerve, go to the corresponding muscles and end in them with motor endings. In the lower part of the pons, fibers are separated from the motor tract to the motor nuclei of the facial nerve of its own and opposite sides, after which the pyramidal tract passes into the medulla oblongata, where it again takes the form of a compact bundle. In the upper part of the medulla oblongata, fibers extend from the pyramidal tract to the motor nuclei of the vagus, glossopharyngeal and hypoglossal nerves. After these bundles depart, the pyramidal tract consists only of fibers connecting the cortex with the nuclei of the anterior horns of the spinal cord. Most of these fibers cross over in the lower part of the medulla oblongata (decmsatio pyramidum)
and passes into the lateral cord of the spinal cord, where it forms
the lateral (pyramidal) corticospinal tract, tractus corticospinalis lateralis.
The fibers of this pathway end in the motor nuclei of the anterior horns of the spinal cord.
A minority of fibers in the region of the medulla oblongata do not form a decussation. These fibers in the spinal cord make up the anterior corticospinal tract, tractus corticospinalis ventralis,
some of the fibers of which end
is formed in the motor nuclei of the spinal cord on its side, and the other part of the fibers crosses through the anterior white commissure and ends in the same nuclei of the opposite side. The anterior bundle can be traced only in the cervical and upper thoracic segments of the spinal cord.
Thus, the pyramidal tract primarily carries out cross-innervation of the muscles of the body, and with unilateral damage to the central neurons of any part, muscle paralysis occurs on the side opposite to the lesion. Such unilateral innervation is not typical for all muscle groups. Most of the muscles, namely the muscles of the eyeball, mastication, facial muscles of the upper part of the face, muscles of the pharynx, larynx, neck, torso and perineum, receive so-called bilateral innervation, i.e. from the central neurons of both their own and the opposite side. This, to a certain extent, ensures the preservation of the innervation of these muscles with unilateral damage to the central neurons.
Unilateral innervation of the muscles of the limbs, tongue and facial muscles of the lower half of the face. In this regard, with unilateral damage to the central neurons of these muscles, a complete loss of the ability to move occurs, i.e. paralysis.
2. The pathways of the extrapyramidal system pass to the anterior horns of the spinal cord outside the pyramidal tracts, through the tegmentum and the reticular formation of the brain stem. The extrapyramidal system includes the following formations: the caudate and lenticular nuclei, thalamus, substantia nigra, red nucleus, hypothalamic formations, cerebellum, inferior olive and nuclei of the reticular formation of the brain stem. Compared to the pyramid, the extrapyramidal system is a phylogenetically older formation, the function of which is to carry out complex unconditioned reflex motor acts based on the experience of the species, while motor conscious cortical activity is based on conditioned reflexes that consolidate individual experience.
The extrapyramidal system provides automatic, without the participation of consciousness, regulation and coordination of muscle tissue tone, contracts or relaxes certain muscle groups, and ensures the readiness of the motor system to perform complex, precise, purposeful actions. Lesions of the extrapyramidal system are manifested mainly by changes in muscle tone and motor activity.
TYPICAL FEATURES OF THE STRUCTURE OF THE CENTRAL NERVOUS SYSTEM
The central nervous system has some specific structural and functional differences in different people. These differences relate to the shape of the brain and its individual formations, size, mass and other indicators.
Thus, the mass of the human brain, as a rule, ranges from 1100 to 2300 g. It should be noted that a large brain mass (within normal limits) does not indicate high intelligence, and vice versa. There is a certain correspondence between the shape of the brain and the shape of the skull. The dolichocephalic, mesocephalic and brachycephalic forms of the skull correspond to a certain position of its sections, formations, grooves, etc. This circumstance is of great practical importance in connection with the possibility of projections onto the outer integument of the head of various nuclei, grooves and convolutions.
MEMBRANES OF THE BRAIN
Dura mater encephali,
adjacent to the inner surface of the skull bones and tightly fused with it in the area of the base and sutures.
The loose connection of the shell with the bones of the cranial vault served as the basis for the allocation of a very narrow epidural space,
which is penetrated by connective tissue fibers, vessels and nerves.
The arachnoid membrane
is adjacent to the smooth inner surface of the dura mater.
The narrow gap between them is conventionally called the subdural space.
In some places, the hard shell forms spurs (shoots) that penetrate between different parts of the brain. Thus, in the longitudinal fissure of the hemispheres there is a crescent-shaped process - the falx cerebrum, falx cerebri.
The upper thickened edge of the falx cerebri, formed by two diverging plates of the dura mater, is adjacent to the sagittal groove of the skull from the cock's crest of the ethmoid bone to the internal occipital protuberance (Fig. 213).
tentorium cerebellum, tentorium cerebelli,
It is a wide fold of the dura mater, which in the form of a gable roof is located in the transverse groove of the brain, separating the contents of the posterior cranial fossa from the occipital lobes. The posterolateral thickened edge of the cerebellar tentorium is fused with the groove of the transverse sinus and the upper edge of the pyramid of the temporal bone. The free edge has a rounded shape. It is stretched between the back end of the free edge
Rice. 213. Meninges of the brain. 1 _ granulation of the arachnoid membrane; 2 - emissary vein; 3 - vein of cancellous bone; 4 - spongy bone; 5 - hard shell; 6 - crossbars of the arachnoid membrane; 7 - perivascular space; 8 - subarachnoid space; 9 - choroid; 10 - arachnoid membrane; 11 - falx cerebri; 12 - superior sagittal sinus; 13 - cerebral cortex; 14 - branch of the cerebral artery; 15,16 - cerebral veins.
the falx medullaris and the posterior oblique process of the sphenoid bone. The free edge limits the notch of the tentorium cerebellum, incisura tentorii,
through which the posterior and middle fossa of the skull communicate.
The cerebral peduncles are located in the area of this notch. In the posterior fossa of the skull, between the cerebellar hemispheres, lies the falx cerebellum, falx cerebelli.
Diaphragm of the sella turcica, diaphragma sellae,
stretched over the sella turcica.
In the middle of the diaphragm there is a narrow hole through which the funnel passes to the pituitary gland. At the apex of the pyramid of the temporal bone, the processes of the hard shell form the trigeminal cavity, cavum trigeminale;
it contains the trigeminal ganglion.
Arteries, veins, nerve fibers and their endings, as well as special channels - venous sinuses (sinuses) pass through the thickness of the hard shell.
Venous sinuses
represent the spaces between the split layers of the dura mater of the brain. Most of them are located near the walls. The venous sinuses receive blood from the veins of the brain and are then discharged into extracranial venous formations, mainly into the internal jugular veins.
The arachnoid membrane of the brain, arachnoidea mater encephali,
in the form of a thin transparent avascular sheet
covers the brain and passes downwards into the arachnoid membrane of the spinal cord. The arachnoid membrane is firmly fused with the dura mater of the brain through special structures - granulations of the arachnoid membrane, and
also at the points where veins enter the venous sinuses.
The arachnoid and soft membranes limit the subarachnoid space filled with cerebrospinal (cerebral) fluid.
This space is penetrated by numerous connective tissue fibers that connect both membranes and fix the blood vessels located here.
The relationships between these membranes are different in the area of various recesses of the brain. The soft membrane covers the brain surface in the depths of the grooves, fissures and pits, and the arachnoid, without following it into the depths of the furrows and fissures, as if bridged from one elevation of the gyrus to another: forming subarachnoid spaces of varying sizes. The largest of these containers are called subarachnoid cerebellocerebral
located between the cerebellum and the posterior surface of the medulla oblongata;
2) interpeduncular cistern, cistema interpeduncularis,
located between the cerebral peduncles;
3) cross tank, cistema chiasmatis,
located in front of the optic chiasm;
4) cistern of the lateral fossa of the cerebrum, cistema fossae lateralis cerebri,
corresponds to the pit and groove of the same name.
The subarachnoid space is common to the brain and spinal cord. The cerebrospinal fluid formed in the ventricles of the brain enters this space through the openings of the fourth ventricle, and is discharged into the venous system through granulations of the arachnoid membrane.
The soft membrane of the brain, pia mater encephali,
tightly adheres to the medulla both on the free surface of the brain and in the depths of the grooves. The choroid plexuses of the ventricles secrete cerebrospinal fluid. In the thickness of the soft shell there are networks of blood vessels and nerves.
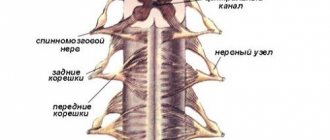
SPINAL NERVES
spinal nerves,
ill.
spindles
are located in the correct order (neuromeres), corresponding to the myotomes (myomeres) of the body and alternating with the segments of the spinal column; Each nerve has a corresponding skin area (dermatome)
A person has 31 pairs of 3 spinal nerves, namely: 8 pairs of cervical, 12 pairs of thoracic, 5 pairs of lumbar, 5 pairs of sacral and 1 pair of coccygeal (see Fig. 267). Each spinal nerve departs from the spinal cord by two roots: the posterior (sensory) and the anterior (motor); both roots are connected to one trunk, trucnus n. spinalis emerging from the spinal canal (through the intervertebral foramen Near and slightly outward from the junction, the dorsal root forms a node, ganglion spindle,
in which the anterior motor root does not participate. Due to the connection of both roots, spinal nerves are mixed nerves: they contain sensory (jaftrenentnmr) fibers from the cells of the spinal ganglia, motor (efferent) fibers from the cells of the anterior horn, as well as vegetative fibers from the cells of the lateral horns, emerging from the spinal cord as part of the anterior horn. roots (Fig. 308).
Vegetative fibers are also present in the dorsal root. Autonomic fibers entering the animal nerves through the roots provide processes in the soma such as trophism, vasomotor reactions, etc.
In cyclostomes (lamreys), both roots continue into separate motor and sensory nerves. In the further course of evolution, starting with transverse fish, the roots come closer together and merge, so that the separate course is maintained only for the roots, and the nerves become mixed. Each spinal nerve, upon exiting the mesenchyme of the foramen, is divided into two parts, respectively. (dorsal and ventral) into two branches:
1) posterior, rumusi dprsgljs, for the autochthonous muscles of the back and the skin covering it, developing from the dorsal part of the myotoma;
2) anterior, ramus ventralis, for the ventral wall of the trunk and limbs, developing from the ventral parts of the myotomes.
In addition, two more types of branches depart from the spinal nerve:
3) for the innervation of the viscera and blood vessels - connecting branches to the sympathetic trunk, rr. communicantes;
4) for the innervation of the membranes of the spinal cord - g. menfngeus, going back through the intervertebral foramen.
vestibulospinal tract
An important link in the coordination of motor functions of the human body is the vestibulospinal tract , tractus ves-tibulospinalis. It connects the nuclei of the vestibular apparatus with the anterior horns of the spinal cord and provides adjustment reactions of the body in case of imbalance. Axons of cells of the lateral vestibular nucleus, as well as the inferior vestibular nucleus of the vestibulocochlear nerve, take part in the formation of the vestibular tract. These fibers descend in the lateral part of the anterior cord of the spinal cord (at the border with the lateral cord) and end on the motor cells of the anterior horns of the spinal cord.
Anatomy of the nervous system pathways
Content
After this, the fibers of the tractus tectospinalis are “directed” through the trunk to the segments of the spinal cord. In the tegmentum of the bridge, this path occupies a dorsomedial position, somewhat ventral to the longitudinal fasciculi. A similar topography is observed in the medulla oblongata, where the tractus tectospinalis is located ventral to the medial longitudinal fasciculus and gradually moves ventrally, approaching the dorsal border of the pyramids. In the spinal cord it is located in the medial part of the anterior funiculus. Gradually, the roof-spinal tract becomes thinner, as some of its fibers end on the motor neurons of the motor nuclei of the cranial nerves in the trunk (roof-nucleus bundle, fasciculus tectonuclearis) and in the overlying segments of the spinal cord. Here, through interneurons, fibers of the tractus tectospinalis influence the alpha small motor neurons of the motor nuclei of the anterior horns.
Motor neurons of the trunk and spinal cord transmit influence through their axons from the integration center of the roof of the midbrain through the cranial and spinal nerves to the innervated skeletal muscles.
Damage to the tractus tectospinalis leads to the loss of starting reflexes to sudden light, sound, olfactory and tactile influences.
Reticulospinal tract
This pathway is considered the most phylogenetically oldest and nonspecific. In this case, the name “tractus reticulospinalis” is understood as a set of efferent fibers starting from various centers of the reticular formation and having functional and topographical features. In a simplified form, the reticulospinal tract can be depicted without decussation, without interneurons, without indicating the specific nucleus from which it originates, and as a single rather than multiple projection (Fig. 18).
Rice. 18. Reticulospinal tracts: 1 - reticular nuclei, 2 - reticulospinal tract, 3 - motor nuclei of the anterior horns of the spinal cord, 4 - spinal nerves
It should be taken into account what the target nucleus is in the spinal cord: in the case of the animal reflex arc, these are the motor nuclei of the anterior horn, and in the case of the sympathetic reflex arc, the intermediate-lateral nucleus of the lateral horn.
In other words, there are several parallel reticulospinal tracts.
The medial reticulospinal tract (tractus reticulospinalis medialis) is the most powerful and longest of the reticulospinal tracts. It begins from the oral and caudal reticular nuclei of the pons and from the reticular nuclei of the medulla oblongata: giant cell and ventral. In the spinal cord, it extends to the sacral segments, gradually thinning and ending segment by segment on the dendrites of the gamma motor neurons of the anterior horns of the spinal cord.
The lateral reticulospinalis tract (tractus reticulospinalis lateralis) begins from the lateral reticular nucleus of the pons, located near the middle cerebellar peduncle (regio parabrachialis). This path, partially crossed, includes the axons of the reticular neurons of the respiratory cord in the spinal cord, where it is located in the lateral funiculus next to the lateral corticospinal tract. Tractus reticulospinalis lateralis has an activating effect on small alpha motor neurons of the anterior horns of the spinal cord. Another part of its fibers ends on the neurons of the intermediate-lateral nucleus of the spinal cord (the center of the sympathetic division of the autonomic nervous system). Therefore, regulation of the organs of “plant life” by the reticular formation becomes possible.
The anterior reticulospinalis tract (tractus reticulospinalis anterior) begins from the tegmental reticular nuclei of the midbrain and pons and, located in the anterior cords of the spinal cord, “reaches” the tenth thoracic segment. This pathway ends at the motor neurons of the anterior horns of the spinal cord.
All reticulospinal tracts are characterized by best expression in the cervical and upper thoracic segments of the spinal cord. More distally, the influence of the reticular formation spreads along the propriospinal tract. In other words, the reticulospinal tract is characterized by the shape of a chain of several sequentially located neurons (polysynaptic organization). Another feature is that the reticulospinal tracts are predominantly uncrossed. All these pathways have an indirect connection with the motor neurons of the anterior horns, since they end on the dendrites of interneurons 7 and 8 of the Rexed plates and through them influence the motor neurons. These influences can be either inhibitory or activating. As a result, the reticular formation, through its reticulospinal tracts and spinal nerves, ensures the tone of skeletal muscles and the performance of complex reflex acts that require the simultaneous participation of many skeletal muscles or even muscle groups (respiratory, grasping movements). Similar relationships exist between the centers of the reticular formation and the nuclei of the cranial nerves.
vestibulospinal tract
This path also refers to very ancient projections in evolutionary terms, closely related to the vestibular analyzer. Tractus vestibulospinalis is involved in the body’s rapid response to such a change in body position in space, which leads to imbalance. In this case, unconditional reflex body movements occur, leading to the fact that a person, having slipped, falls on his outstretched arms and does not hit his head or torso.
This path begins from the lateral vestibular nucleus (Deiters nucleus) (nucl. vestibularis lateralis), located in the tegmentum of the bridge near the border of the latter with the medulla oblongata (Fig. 19).
Rice. 19. Vestibulospinal tract: 1 - vestibular nuclei, 2 - vestibular tract, 3 - motor nuclei of the anterior horns of the spinal cord, 4 - spinal nerves
According to a number of researchers, the tractus vestibulospinalis also includes axons of neurons whose bodies are located in the inferior vestibular nucleus (Roller’s nucleus). The latter is located next to Deiters' nucleus, but somewhat more caudally. The Deiters nucleus has an indirect effect (in particular, through the alpha motor neurons of the motor nuclei of the anterior horns of the spinal cord) on the extensor muscles and is thus a kind of antagonist of the red nucleus. In the medulla oblongata, the vestibulospinal tract is located dorsal and lateral to the pyramids, and in the spinal cord - on the border of the anterior and lateral cords (here it is penetrated by fibers of the anterior roots of the spinal nerves). The path is mostly uncrossed.
Olivespinal tract
Tractus olivospinalis is involved in the unconditioned reflex maintenance of neck muscle tone and in performing movements designed to maintain body balance. This path is relatively young in evolutionary terms, like the olive nucleus (nucleus olivaris) of the medulla oblongata, from which it begins. The olive nucleus has a regulatory influence on the cerebellar hemispheres (cortex and dentate nucleus), the red nucleus and the cortex of the frontal lobe of the cerebral hemisphere.
Axons of neurons nucl. olivaris as part of the tractus olivospinalis reach the sixth cervical segment of the spinal cord, ending segment by segment on the alpha motor neurons of the motor nuclei of the anterior horns on their side of the body (Fig. 20).
Rice. 20. Olivospinal tract: 1 - nuclei of the inferior olive, 2 - olivospinal tract, 3 - motor nuclei of the anterior horns of the spinal cord, 4 - spinal nerves, 5 - neck muscles
The axons of these motor neurons as part of the spinal nerves reach the neck muscles, which innervate them. In the spinal cord, the olivospinal tract is located in the anteromedial part of the lateral funiculus.
3.2. Pyramid paths
These pathways, collectively called the “pyramidal system,” are involved in the conscious control of skeletal muscle function (stimulating or inhibiting contraction). In particular, it is possible to perform voluntary movements characterized by complexity and accuracy. The pyramidal system consists of two pathways: the corticospinal tract (tractus corticospinalis) and the corticonuclear tract (tractus corticonuclearis). The pyramidal system received its name due to the fact that the tractus corticospinalis “passes” through the pyramids of the medulla oblongata. It is clear that the name is not very good, since the main thing here is not topography, but function.
Corticospinal tract
This pathway conducts volitional motor impulses that allow control of skeletal muscles innervated by spinal nerves, i.e. muscles of the limbs, trunk and neck. The corticospinal tract also conducts impulses that can inhibit the activity of motor neurons in the anterior horns of the spinal cord.
VK
Buffer
Corticocerebellar pathway
The functions of the cerebellum, which is involved in coordinating movements of the head, trunk and limbs and is in turn connected with the red nuclei and vestibular apparatus, are controlled from the cerebral cortex through the bridge along the corticopontocerebella tract , tractus corticopontocerebellaris. This pathway consists of two neurons. The cell bodies of the first neuron lie in the cortex of the frontal, temporal, parietal and occipital lobes. The cells of the pontine nuclei with their processes constitute the second neuron of the corticocerebellar tract.