Bone marrow is soft, spongy tissue that is found in some bones, including the femur. People with certain blood disorders may need a transplant, which replaces damaged cells with healthy ones. A bone marrow transplant can be a lifesaver for people with diseases such as lymphoma and leukemia, or when intensive cancer treatment has damaged blood cells. The transplant is an intensive procedure and recovery can take a long time.
Transplant rejection reaction
In patients who have undergone allogeneic bone marrow transplantation
, that is,
a transplant rejection reaction
. The greater the genetic differences between the donor and recipient, the higher the likelihood of developing this condition. It develops when the donor's immune T cells begin to attack the body and cause inflammation. The rejection reaction can be acute or chronic.
Transplant rejection reaction is NOT
occurs when a patient is transplanted with his own stem cells, or if the donor is a twin.
Rejection occurs in the first three months after transplantation, but rarely occurs later. It usually manifests itself through the following symptoms:
During an allogeneic bone marrow transplant, doctors always take measures to avoid rejection. Sometimes they remove the T cells before transplantation, or prescribe medications that suppress their activity. There is no single protocol for preventing a reaction, and depending on the individual patient, doctors may prescribe different combinations of medications.
If a rejection reaction occurs, doctors prescribe corticosteroids
, which suppress the immune system and prevent inflammation from developing.
- Rash, burning, and redness of the skin on the torso, palms, or soles of the feet. The skin may blister. Nausea, vomiting, abdominal cramps, loss of appetite and diarrhea. Yellowing of the skin or eyes.
Patient without a head
A team of researchers reported successful restoration of motor function in animals with severed spinal cords. Among the authors of the publication is Sergio Canavero, the same Italian neurosurgeon who has been promising to transplant a human head onto a donor’s body for many years. About the history of this project and how to treat Canavero's promises, at the request of N + 1
says Pyotr Talantov, author of the just published book “0.05. Evidence-based medicine from magic to the search for immortality."
Head transplantation is a favorite plot point in science fiction films and science news sections. And it’s not just the incredible technical complexity of the transplant. On the one hand, the thought of living with someone else's body excites the imagination, affects the sense of identity and makes us think about who we are. On the other hand, it opens the door to immortality. If we ever learn to discard our bodies like worn-out clothes, we will no longer be afraid of old age and death.
All this dooms any news about a head transplant to heated discussion. For some time now, the main newsmaker in transplantology has been Sergio Canavero, who has been promising to write his name in the history of surgery with this operation for several years. If you take his word for it, all the necessary technologies have been created and the only thing is to assemble a team of experienced surgeons and find a lot of money. But the deadlines once named by Canavero have passed, and even the first potential patient managed to change his mind. Maybe it’s true, as the skeptics say (and they are the majority), we are still too far from planning such an operation seriously?
Any organ transplant operation requires solving several problems at once, each of which, if not eliminated, will lead to failure. In the case of a head transplant, protecting the brain from ischemia (decreased blood circulation) is critical - even a few minutes of ischemia will lead to irreversible changes in the brain and the death of the recipient’s personality. Apparently, this is why the first attempts to transplant a dog's head onto a donor body at the beginning of the 20th century were unsuccessful.
Restore blood supply
Attempts to maintain life in a head separated from the body were made by our compatriot Sergei Bryukhonenko. In the 1930s, while working at the Institute of Experimental Physiology and Therapy, he created one of the first artificial blood circulation devices, called an autojector. The twenty-minute film "Experiments in the Revitalization of the Organism" shows a dog's head severed from its body. She is attached to the device and remains alive - she reacts to tickling with a feather, blinks and licks her lips. The voiceover says that the head connected to the autojector remains in this state for many hours. However, later witnesses admitted that it was possible to maintain the dog’s heads in this state for only a few minutes. And the famous scene from the film is now considered a falsification.
Bryukhonenko's experiments inspired surgeon Vladimir Demikhov to even more daring experiments. He transplanted the upper torso—the head and front legs—of puppies onto the bodies of larger dogs. Demikhov's method made it possible to perform the operation without ischemia threatening brain death. The animals survived for up to twenty-nine days, while moving, responding to stimuli and drinking water. But Demikhov remained in history not so much because of this strange experiment, but because he was the first in the world to transplant a heart, lungs and liver from one animal to another. Thanks to his developments, successful human-to-human heart transplantation became possible in 1967. The surgeon who performed it, Christian Barnard, repeatedly came to Demikhov’s laboratory and subsequently called him his teacher.
Scheme of dog head transplant using Vladimir Demikhov's technology
Public domain
Share
Vladimir Demikhov (right) during surgery
Public domain
Share
An animal after an operation to transplant the head of a living dog to another dog
Public domain
Share
Demikhov's dogs died from an immune process called transplant rejection. In the absence of effective immune suppression technologies, this outcome was inevitable. In head transplants, the rejection reaction can be directed both at the donor body and, more likely, at the recipient's head. Even now, despite immune-suppressing medications, acute rejection occurs in 10 to 30 percent of liver and kidney transplants. And if kidney rejection leaves the patient the chance to wait for a new donor organ on an artificial kidney, then head rejection certainly threatens death.
Suppress rejection
Methods of immune suppression that appeared in the mid-20th century contributed to the relative success of the experiments of the American neurosurgeon Robert White. He took on an even more difficult task: transplanting the isolated brain of one dog into the skull of another. Six operations were relatively successful: the nervous systems of the donor brain and the recipient body were not connected, but the brain was effectively supplied with blood - this was confirmed by sufficient electrical and metabolic activity, after the operation the animals lived for up to two days.
Subsequently, White transplanted monkey heads: within a few hours after the operation, they could chew, swallow food, bite and follow moving objects with their eyes. However, they did not live long: the blood supply was still not efficient enough. And although hyperacute rejection of the transplanted heads was prevented, White achieved this with such high doses of immune-suppressing substances that they themselves contributed to the death of the animals.
Over time, White planned to move on to operations on humans, trained on corpses in the morgue and dreamed of transplanting Stephen Hawking's head onto a donor body. Fortunately for the latter, he was not interested in this opportunity and outlived White by eight years.
A-B - four mice of different colors before a head transplant operation using the technology of surgeon Ren Xiaoping; C-D: white mouse with a black head and vice versa; E - black mouse with a gray head
Dr. Xiaoping Ren et al. / CNS Neuroscience & Therapeutics
Share
A - vessels for blood transfusion; B — mice before surgery (from left to right: blood source, donor, recipient); C—mouse—source of blood and mouse donor; DE - mice after transplantation
Dr. Xiaoping Ren et al. / CNS Neuroscience & Therapeutics
Share
Chinese surgeon Ren Xiaoping was able to achieve greater life expectancy for animals. He changed the operating protocol, ensuring that sufficient blood pressure was maintained in the recipient's head vessels throughout the operation. In 2015, he reported on hundreds of mouse head transplants, half of the animals survived more than 24 hours after surgery, with a maximum survival rate of up to six months.
Ren also suggested changing the level at which the head was separated from the body. He proposed making the incision high enough so that the brain stem with the centers for regulating breathing and blood circulation remains on the donor body, which as a result will be able to breathe independently and be supplied with blood without the help of life support machines.
Operation on a person
Around the same time, Sergio Canavero appeared on the scene. A previously little-known Italian neurosurgeon said that he could solve the main problem of a head transplant - restoring the integrity of the spinal cord. So far, all attempts to fuse the spinal cord after the incision have been unsuccessful. There are several directions in which research is going, but they are all at an early stage.
Attempts are being made to stimulate the regeneration of neurons using electrical impulses and to use stem cells. Interesting experiments with computer interfaces: one device reads brain signals and transmits it to another, located below the site of spinal cord damage, which deciphers them and transmits them to motor neurons. Although all of these technologies sound promising, none have yet achieved complete success, even in animal experiments. Moreover, we are not talking about results suitable for people: there are thousands of patients with damaged spinal cord in the world, and if there is an effective technique, there will definitely be someone to study it on long before head transplant operations.
Canavero called his technology GEMINI. It consists of a very precise and thin section of the spinal cord and the use of polyethylene glycol as a substance that “glues” ruptured neuronal membranes. Canavero said that all the technologies necessary for a successful head transplant have already been created and he will perform the operation on a person in the very near future. According to his estimates, it should have cost about 15 million euros, lasted more than 36 hours and involved 150 doctors.
Soon the first patient appeared. Canavero announced that no later than 2021 he will transplant the head of 33-year-old Russian IT specialist Valery Spiridonov, who suffers from spinal muscular atrophy, a rare hereditary disease accompanied by the loss of motor neurons and a sharp decrease in muscle mass, onto a donor body.
Although Canavero claimed that the operation had a success rate of at least 90 percent, he did not have the minimum necessary evidence obtained from previous animal experiments. The only evidence at that time that GEMINI could, in principle, work was the publication of its Korean colleague Si Yun Kim. He reported that polyethylene glycol led to a partial restoration of motor function in mice with a severed spinal cord. At the same time, the attentive reader will find that although the experimental mice recovered slightly better, the difference with the control group was not statistically significant, that is, it could well be explained by chance.
Pros against
Despite Spiridonov's readiness and Canavero's enthusiasm, the possible operation raised many questions and sharp criticism from most professionals. The risk of death of the patient during the operation or shortly after it was extremely high: most animals died in the first days after transplantation. The risk of transplant rejection was also great; it could only be reduced by powerful lifelong immunosuppressive therapy, itself a source of fatal risk. The chances of gaining mobility were ephemeral and unconfirmed. But the risk of difficult-to-treat neuropathic pain was very real. Canavero also proposed to solve this problem surgically - by destroying the part of the brain responsible for transmitting the emotional component of pain, which causes the suffering associated with it.
There would probably be other problems that we are not yet aware of. But even the above is enough to understand: the balance of potential benefits and harms is unlikely to be in favor of the operation. The conclusion remains the same even when considering patients facing imminent death.
Some skeptics recalled the story of another transplant surgeon, Paolo Macchiarini, who worked first at Karolinska University and then at Kazan Federal University. He claimed that he had developed a technique for transplanting an artificial trachea containing stem cells - supposedly the organ takes root and does not cause an immune response in the patient’s body. Later it turned out that the technique had not been tested on animals, did not work in any case, and Macchiarini condemned several patients to severe surgery and the suffering associated with it without the slightest hope of improvement.
Another, perhaps the most important of the critics' arguments, was of an absolutely practical nature. The demand for donor organs significantly exceeds the supply. On average, 20 people die every day without waiting their turn. However, the situation is not getting better: the list of people waiting for transplantation is growing faster than the number of available organs. Is it reasonable to use a donated body to save (with a slim chance of success) one life, rather than using those organs to save and improve the lives of 10-15 patients?
Modest result
However, time passed, and conversations remained conversations. Funded by the Chinese government, Canavero works with Ren Xiaoping. The recent publication is the result of their collaboration. But we are no longer talking about a head transplant: the work is being carried out as part of a project to treat spinal cord injuries. Although Canavero sent out triumphant press releases in late 2021 about the successful head transplant, the operation was performed on a cadaver. Meanwhile, Valery Spiridonov lost interest in the idea of becoming the first volunteer for such an operation, got married and moved to live in Florida. According to foreign media reports, his beautiful wife gave birth to a healthy child.
Expert opinion
I would approach this work with caution. Almost two years ago, Canavero’s group published articles in which they said that it is now possible to perform a head transplant operation and there is a test subject - that Russian programmer. And only now the first article appears, which substantiates what supposedly could have been realized two years ago. In standard practice, it happens the other way around: first you describe the theoretical basis, then conduct experiments in vitro
, then
in vivo
, and only after that you start talking about the possibility of operations on humans. The theoretical framework on which this study relies is insufficient. If you look at the list of references in the article, it is very small, and mostly the authors refer to themselves, to their research, and this is always alarming, as is the size of the article.
The magazine itself, let's say, is not the top one in the world. If this article had been published with a reference list of 60-100 names in Cell
or
the Lancet
, I would have more confidence in it.
It is important that Canavero and his colleagues were the initiators of the idea of using polyethylene glycol - it supposedly prevents the formation of scar between nerve tissues and promotes recovery. But there is no independent confirmation of this.
And this statement itself is doubtful: nerves do not grow into each other not only because a scar is formed there, but also because they have, in principle, a low regenerative ability. If we consider that the same article itself states that no significant difference in scar formation could be detected, then the mechanism of action of polyethylene glycol becomes completely unclear.
Many groups are working on methods to restore the spinal cord. In particular, electrical stimulation produces interesting results; there is evidence that electrical stimulation below the level of damage leads to increased growth, moreover, there are cautious attempts to use this in humans. There is Martin Schwab's research group that is studying the capabilities of the Nogo-A family of proteins for spinal cord cross-linking. But these works last for decades. It doesn’t happen that you wrote a four-page article and you can already use it on a person.
I'm not saying that the Canavero group is cheating. But longer studies and evaluation on large groups of animals are needed. And it’s strange that they start with the spinal cord, and not with simpler models, such as nerves.
Alexey Kashcheev, neurosurgeon, employee of the Scientific Center of Neurology
Share
However, Canavero is unlikely to be satisfied with modest work on everyday medical problems. In recent interviews, he claimed that a head transplant was a thing of the past for him. Now Canavero is going to move on to the second stage of the project - transplanting the brain into a donor body and promises to perform this operation on humans in the next 3-5 years. I would like to believe that this time he will limit himself to corpses.
Peter Talantov
Pre-order the book “0.05. Evidence-based medicine from magic to the search for immortality" can be made on the publisher's website, discount code - 005 The book is published by Corpus publishing house with the support of the Evolution educational foundation.
Literature
Sergio Canavero.
HEAVEN: The head anastomosis venture Project outline for the first human head transplantation with spinal linkage (GEMINI) // Surg Neurol Int. 2013; 4(Suppl 1): S335–S342. Allen Furr, Mark A. Hardy, Juan P. Barrett, John H. Barkerd. Surgical, ethical, and psychosocial considerations in human head transplantation // Int J Surg. May 2021; 41: 190–195. Nayan Lamba, Daniel Holsgrove, Marike L. Broekman. The history of head transplantation: a review // Acta Neurochir (Wien). 2016; 158(12): 2239–2247.
Shuai Ren et al. Reconstruction of the spinal cord of spinal transected dogs with polyethylene glycol, 26-Mar-2019;10:50
Share
Physiotherapy during rehabilitation after BMT
Physical exercise plays an extra large role in the rehabilitation process. Due to long-term treatment, most patients experience severe fatigue. However, constant lying down has a negative effect on all body systems and slows down the process of restoring health.
A patient recovering from a bone marrow transplant needs to walk more than 60 meters
and do physical exercise.
Patients who cannot withstand this type of exercise consult with a physical therapist to evaluate pain, muscle weakness, or fatigue. The doctor may change the exercises or suggest an alternative so that the body still receives the necessary daily load.
This can be active or passive exercises while lying down, the use of auxiliary materials (pillows, braces), massages or gymnastics with the help of a nurse. An exercise bike or portable pedals can be placed in the room.
Preventing Infections After Bone Marrow Transplant
- In cancer centers that specialize in BMT, bone marrow transplant patients are placed in sterile rooms with air filtration systems, such as HEPA filters. They do not allow viruses, bacteria and fungi into the room and allow you to avoid dangerous infections.
After surgery, doctors also prescribe antibiotics. This further reduces the risk of infection. After discharge, patients should remember the following precautions:
- Wash your hands frequently using antibacterial soap or alcohol-based sanitizer; Avoid sick people who have recently been ill or have been in contact with sick people; Wear a protective mask.
Method capabilities
According to statistics, more than 126 organ transplant operations are performed annually in the world. Transplant operations are performed to save the lives of patients whose organ functions are impaired or lost. About 41% of the total structure of all operations is kidney transplantation. In 2nd and 3rd place are liver and heart transplants. Not only people, but also genetically modified pigs can act as donors.
American scientists from the company eGenesis, which specializes in biotechnology, modified the animal's genome, bringing it closer to the human model. At the same time, specific viruses that interfered with operations were removed from the genome of pigs. The only problem that has not been completely resolved is the possibility of rejection of a foreign organ.
Despite successful transplantation of many internal organs, brain transplantation remains a difficult task. The brain is a highly organized structure. The main problem that arises during a brain transplant operation is the inability to connect the crossed nerve fibers of the spinal cord. As a result, the body remains immobilized because it does not receive commands from the brain centers.
The continuity of the nerve pathways along which impulses are transmitted from the motor centers to remote parts of the body (limbs, torso) makes it possible to perform voluntary movements. If the integrity of the spinal cord is damaged as a result of an accident or other injury, a person loses the ability to move and becomes disabled.
Realistic human brain transplant operations involve replacing individual sections of damaged brain matter; perhaps in the near future, in a similar way, it will be possible to eliminate disorders associated with neurodegenerative, ischemic, necrotic processes in the nervous tissue. The technology is already being used to treat dementia, epilepsy and multiple sclerosis.
Low blood counts during rehabilitation
Patients usually suffer from anemia
and
thrombocytopenia
. This manifests itself as increased fatigue and a tendency to bleed. With the restoration of the bone marrow, these indicators will return to normal, but in the meantime the patient’s condition is being maintained with doctors.
Anemia is less well tolerated by older patients, people with chronic obstructive pulmonary disease or cardiovascular disease.
A low platelet count leads to frequent bleeding. If the level is below 5,000 /ml, a platelet transfusion from the blood bank is performed.
Read: How to deal with chemotherapy side effects?
Digestive system problems
During the rehabilitation period, patients often suffer from gastroenterological symptoms - diarrhea, nausea, vomiting. They can be caused either by chemotherapy or be a symptom of an implant rejection reaction.
To treat symptoms, doctors usually prescribe several medications at once:
- medications to relieve symptoms; medications that treat the cause of symptoms.
In severe cases, the patient may have difficulty eating, leading to unwanted weight loss and nutritional deficiencies. Such a patient should consult a nutritionist. A doctor of this specialty will create a special diet that will be easier for the body to tolerate and sufficiently provide it with energy and nutrients.
Neurological rehabilitation after bone marrow transplantation
Neurological problems are a common side effect of many medications a patient takes during the post-bone marrow transplant period. Patients may suffer from pain, fatigue, memory and attention problems, mood swings, etc. Often these symptoms go away over time. In other cases, the patient will be able to improve his condition with the help of neurological rehabilitation
.
- splints
and
orthoses
help - special orthopedic devices for fixing parts of the body in the required position. Passive orthoses provide support while at rest, while dynamic orthoses use springs or tension to facilitate weak movements of the patient. In addition, these devices reduce the risk of injury during movement. Depending on the symptoms, doctors may prescribe various medications - antidepressants, anticonvulsants and painkillers. Compression stockings and bandages can help relieve leg pain. They compress blood vessels and help normalize blood pressure.
- Many patients benefit from massage and acupuncture. Physical activity allows patients to relieve stress and be more alert. In case of memory impairment, the doctor will teach the patient mnemonic techniques
that will help to be less forgetful. These include using lists, calendars, and visual and auditory reminders to train the brain to pay more attention to detail. Energy conservation and prioritization techniques will help patients be more efficient by managing their energy more efficiently.
Respiratory problems
Diseases of the respiratory system are common among patients who have undergone a bone marrow transplant. Doctors do oximetry
—measuring oxygen levels in the blood—at rest and during exercise.
Treatment for the patient depends on the specific disease.
For milder syndromes, the patient may be shown exercises to strengthen the respiratory muscles, increase chest mobility, and learn effective techniques for clearing the respiratory tract.
Problems with the cardiovascular system
Medicines used during recovery from a bone marrow transplant can weaken the heart muscle. Doctors carefully monitor heart rate and blood pressure during physical therapy and warn patients against exercise that will put too much strain on the heart.
- A Canadian study found that despite side effects following a bone marrow transplant, 81% of patients were satisfied with their quality of life and 94% would recommend the procedure to others with the same condition.
History of experiments
The idea of head transplantation was first implemented by the American physiologist Charles Guthrie, who in 1908 grafted the head of one dog onto the body of another. The experiments were continued by the Soviet doctor, one of the founders of transplantation, Vladimir Demikhov.
One of the dog heads implanted by Demikhov lived for 32 days, maintaining vital functions and reactions to external stimuli. In 1970, American scientists led by neurosurgeon Robert White transplanted the head of a monkey, attaching it to the body of another individual.
In 2013, Italian doctor Sergio Canavero announced that a human head transplant is possible - the problem of connecting spinal cord tissues was solved with the help of fusogens (glycoproteins that facilitate intercellular fusion, ensuring the connection of cells and cell membranes). A successful neurosurgical intervention, when a person’s head was transplanted, took place in 2017.
The operation took place in China under the leadership of Canavero. During the intervention, the head of a deceased person was transplanted onto the body of a corpse. During the transplant, doctors managed to connect the nerve fibers of the spinal cord and blood vessels. The success of the operation, according to Canavero, is confirmed by a postoperative experiment - electrical stimulation of nerve fibers shows the conduction of impulses in the nervous tissue.
The achievements of the Italian doctor are questioned by some colleagues. For example, English neuroscientist Dean Burnett argues that, despite the scientific value of the methods that Canavero uses in his work, the result of the operation did not confirm the possibility of the life of an organism with a fully functional, transplanted organ.
As numerous experiments have shown, it is possible to transplant a head, but the life expectancy of a living creature after surgery is very short, which allows us to draw conclusions about the futility and failure of such neurosurgical interventions.
Skin care during rehabilitation after bone marrow transplantation
Skin care after BMT is extremely important, especially for patients who lead a predominantly sedentary lifestyle. It is necessary to avoid the occurrence of bedsores, diaper rash, skin disorders, etc.
Basic skin care recommendations are:
- Use moisturizing and absorbent creams; Use disinfecting creams for wounds, scratches, irritations and rashes; Consume the amount of protein recommended by a nutritionist;
- Take vitamin C and zinc; Lie alternately on your back and side, changing position at least every two hours; Avoid increased pressure on the heels, sacral spine, elbows, back of the head, ankles and hips while lying down;
It is important to help the patient use the toilet normally. The patient may have difficulty walking to the toilet or using the toilet on his own.
When can you go home?
The doctor will discharge the patient after the bone marrow transplant, when the patient's health is partially restored. Main criteria for discharge:
- No fever for 48 hours; The patient has not felt nauseous after taking medications within the last 48 hours; Nausea, vomiting, and diarrhea are controlled with medications; Neutrophil level at least 500 to 1,000/ml; Hematocrit 25%-30%; Platelet level – 15,000-20,000/ml; Availability of a person who will care for the sick person at home; The house is prepared for the patient's arrival, in which sharp and slippery objects have been removed and completely disinfected.
After the patient is discharged from the clinic, it is necessary to undergo a weekly examination
. It includes an assessment of how well the transplant has taken root, an assessment of side effects from drugs, and a blood test.
Those who have undergone an allogeneic transplant are advised to live close to the clinic for the first 100 days, and always wear gloves and a face mask when away from home.
On the 100th day after bone marrow transplant, a bone marrow biopsy and aspiration, a slit-lamp examination of the cornea, and a Schirmer test are performed.
What questions often concern patients undergoing bone marrow transplantation?
| What diet should you follow after a bone marrow transplant? | People recovering from a bone marrow transplant should consume 50-60% more calories and twice as much protein as the average person of the same age and gender. This diet should be followed for several months. It will help the body recover faster and resist infections. |
| Do I need to get all my vaccinations again after a bone marrow transplant? | Due to the destruction of the previous bone marrow, the patient loses the immunity acquired throughout life. This means that vaccinations given in the past no longer work, and a person may again catch an infection that they had as a child. Repeated vaccination is not carried out immediately, as the body needs time to recover. This issue should be discussed with your doctor. |
| Is it possible to get pregnant after a bone marrow transplant? | High doses of chemotherapy given before a bone marrow transplant may reduce the chance of subsequent pregnancy. The likelihood of becoming pregnant depends on the total dose of chemotherapy and radiation, as well as the age of the mother. There is an increased risk of miscarriage, premature birth, and having a low birth weight baby. However, among patients under 25 years of age, 79% managed to restore reproductive function . Women who wish to become mothers after a bone marrow transplant should consider egg freezing before treatment. |
| Does your blood type change after a bone marrow transplant? | This usually does not happen, but in rare cases a patient's blood type may actually change. |
| What disability group will a person have after a bone marrow transplant? | The bone marrow transplant procedure is not an indication for disability. Establishing a disability group depends on the individual consequences of treatment if a person loses the ability to self-care and perform work duties. These side effects are strictly individual. |
Ethical considerations
Ethical issues in connection with operations where embryonic nerve cells are transplanted into another person include the specifics of obtaining donor tissue. Currently, embryonic nerve tissue is obtained during legal abortions. The shortage and order of distribution of donor tissues are also associated with various violations and manipulations of responsible officials.
A brain transplant operation costs a lot of money, which makes the procedure inaccessible to most people - how many patients can receive adequate medical care and move, walk and talk normally after a stroke determines the amount of financial well-being.
With the commercialization of transplantation, human organs and tissues have become commodities. The person whose brain is transplanted loses his identity. In turn, the recipient’s personality is also transformed, transformed. If the entire brain is transferred, we are talking about preserving the personality in another body.
The answer to the question of whether it is possible to completely transplant an entire brain is yes. However, the consequences of such surgical intervention are not predictable, and the positive results are short-term.
The story of a patient who underwent a bone marrow transplant
Valentina is a MediGlobus patient who contacted us in 2019. For 10 years she battled chronic myeloid leukemia. As a result of long-term therapy, the medications stopped helping, and the woman needed treatment that was not available in her home country.
The University Hospital of Navarra agreed to accept the woman, where they helped find a suitable donor from the International Registry. Operation was successfully completed.
After the bone marrow transplant, Valentina spent 5 months in Spain. She stayed in a special ward for patients after BMT, which guarantees sterility and the absence of pathogens. Thanks to the comprehensive work of doctors from various specialties, the rehabilitation went well, and the woman was able to return home without serious health complications.
Read: The story of a patient who underwent BMT in Spain
Avatar and others
Let's remember the classic movies. "RoboCop", which "killed" the bad guys, was a robot with the brain of a person (a murdered policeman), practically invulnerable. In the films "Surrogates" and "Avatar", the artificial body was remotely controlled by thought. The human operator is in comfortable conditions (say, sitting in front of a monitor with a can of beer), but his consciousness is “included” in his cyber double. And through the so-called “brain-computer interface” he moves it as he wants. If he wants, he goes to work, if he wants, he runs into battle and frees the hostages. An avatar, instead of a person, can put out a fire, eliminate a nuclear power plant accident, and wander around other planets.
Article on the topic
The brain rules! In 15 years we will control a computer with our thoughts
“Some technologies already exist, others can be created in 5-10 years,” says Dmitry Itskov. — The TELESAR V robot has been developed at Keio University in Japan. Everything it sees and hears is transmitted to the operator, who wears a helmet with three-dimensional image displays. The robot is also equipped with sensitive fingers that transmit tactile sensations.”
Russia also has developments in the field of robotics. Several institutes are conducting research on controlling a computer “with the power of thought.” And doctors are working on reproducing the human body, growing organs for it. “An artificial bladder, mammary gland, blood vessels, and trachea have already been obtained. You can grow almost any organ, even the most complex,” says Dmitry Shamenkov, director of the Center for Cellular and Biomedical Technologies of the 1st Moscow State Medical University. “There are tissue printers: a 3D model is created, it is seeded with cells, and the organ is grown.”
The Institute of Synthetic Polymer Materials of the Russian Academy of Sciences has created a neural-like system capable of recognizing odors - an “electronic nose”.
So, constructing a body with a humanoid skeleton, a set of muscles and sensors is not a problem for modern science. It is possible, after all, to make a primitive iron robot powered by batteries. But how to “include” human consciousness or transplant the brain? “It is clear that the preservation of personality, our “I”, is associated with the preservation of memory. The problem of creating artificial memory, although complex, is solvable, says Alexander Frolov, head of the laboratory of the Institute of Higher Nervous Activity and Neurophysiology of the Russian Academy of Sciences. “One can imagine a variant of “rewriting” consciousness, when a prosthesis imitating a neural network is implanted into the brain instead of the damaged area and then included in a distributed memory system.”
Which foreign clinics perform TCM?
One of the main advantages of treatment abroad is the clinics’ access to the International Bone Marrow Donor Bank. This saves the lives of people who do not have compatible donors among their relatives, or who cannot undergo the procedure in hospitals at home.
- University Hospital of Navarra; Liv Ankara Clinic; Koç University Hospital;
- Chaim Sheba Medical Center; University Hospital Cologne; Hadassah Clinic.
Read: Where is bone marrow transplant performed abroad and how much does it cost?
Summary
The rehabilitation period begins immediately after the bone marrow transplant.
During the first 2-6 weeks, the new stem cells take root and begin to divide and form healthy blood cells. Until the blood counts are restored, the patient will need to remain in the hospital. In cancer centers that specialize in BMT, bone marrow transplant patients are placed in sterile rooms with air filtration systems, such as HEPA filters. They do not allow viruses, bacteria and fungi into the room and allow you to avoid dangerous infections. During the rehabilitation period after a bone marrow transplant, doctors pay great attention to the prevention of severe complications: graft rejection, infections, diseases of the respiratory and circulatory systems. The consequences that occur after a bone marrow transplant depend on the individual reaction of the body. Physical exercise plays a very important role in the rehabilitation process. A patient recovering from a bone marrow transplant must walk more than 60 meters and exercise daily. Bone marrow transplantation often leads to changes in the existing lifestyle, but does not necessarily affect the quality of life. It is important to give your body time to recover from intense stress and support it with healthy exercise, a healthy diet and an optimistic mood. Bone marrow transplantation for foreigners with access to the International Donor Bank is available in leading cancer centers in Turkey, Spain, Israel and Germany. Contact the medical coordinators of the international MediGlobus platform, and we will be happy to help you organize treatment abroad. Our company cooperates with reliable clinics and global specialists in performing TCM.
Indications for transplantation
Any transplant operation involves a long recovery and lifelong use of maintenance medications. When deciding on the advisability of an operation, the doctor takes into account the prospects and consequences, determines the relationship between the advantages and disadvantages of the procedure for the patient. Brain transplantation is carried out within the framework of fragmentary engraftment of the neural tissue of the embryo.
The main goals of the intervention: ensuring the integration of embryonic tissue with the recipient’s brain matter, increasing the viability of the neurotransplant. Research shows that a fragment of embryonic neural tissue placed in the cortical layer of an animal’s brain has the ability to grow, fill the defect cavity and differentiate, which is accompanied by the formation of nerve connections with the cells of the recipient’s medulla.
Over time, the engrafted fragment is penetrated by blood vessels, which ensures normal nutrition - the supply of oxygen and glucose. The viability of the graft is confirmed not only by the formation of a nourishing vascular network and the restoration of structural connections between neurons. Scientists noted in recipients the presence of initial innervation of the medulla and corresponding vascular reactions (changes in tone).
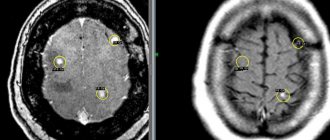
Transplantation of embryonic nervous tissue into the cortical parts of the brain is used to treat intracerebral hematomas of non-traumatic origin that occur in humans due to impaired cerebral blood flow. Hemorrhagic stroke accounts for about 10-15% of the overall structure of stroke. Only about 40% of patients survive 1 year after an episode of hemorrhagic stroke.
In many patients in the post-stroke period, the functions of the central nervous system are impaired, which manifests itself in the inability to speak, move normally, and interact with people around them and the world. Treatment of hemorrhagic stroke usually involves surgical removal of the hematoma and elimination of compression of the medulla. One of the methods of reconstructive surgery is the transplantation of embryonic nervous tissue into a pathological focus where damage to the recipient’s brain matter occurred.
Studies show that if embryonic tissue is transplanted into the brain of another person, it is possible to restore the functions of the damaged fragment of the brain, which reduces the mortality rate and reduces post-stroke neurological disorders. How successful the operation will be depends on the individual characteristics of the recipient’s body, the volume and degree of damage to the brain matter.
Since 1985, successful experiments have been conducted to treat Parkinson's disease using transplanted embryonic nerve cells. Doctors transplant cells from the embryo into the brain, where they subsequently proliferate, differentiate, and become fully integrated into the recipient's medulla. Neurons of the transplanted fragment form synaptic and non-synaptic connections with the recipient's nerve cells, release neurotransmitters, and exhibit trophic and growth characteristics.
Intracerebral systems created in the brain through embryonic cell transplantation make it possible to normalize impaired brain functions, which leads to a reduction in the manifestations of neurological deficits. Neurotransplantation is also carried out to eliminate the consequences of damage to central nervous system tissue of ischemic and traumatic origin.
Embryonic nerve cells are used to treat epilepsy. Patients after transplantation experience restoration of impaired central nervous system functions to varying degrees. Statistics show that patients with drug-resistant (resistant to drug therapy) form of epilepsy experience regression of symptoms for a period of up to 2.5-3 years with a reduction in the number of attacks.
In parallel, there is an improvement in cognitive functions and stabilization of neuropsychological and neurological status. Positive results are confirmed during examination in EEG (electroencephalography) format. Doctors attribute the positive clinical effect to the neurotrophic effect of the neurotransplant on the patient’s central nervous system.