Cavernous angioma is a benign neoplasm in the brain, which consists of pathologically developed blood vessels, which determines the nature of the course of the disease. In most cases, it is a congenital defect of the blood flow system. Unlike vascular malformations (improper connection of arteries and veins) of another type, the pathology is usually asymptomatic. Cavernous angioma is often discovered incidentally during an MRI or CT scan ordered for another reason.
Features of the pathology
Cavernoma is a brain pathology that manifests itself with a variety of nonspecific symptoms, which makes diagnosis and differentiation difficult. Clinical manifestations are observed in 4-5% of cases. Most patients have no clinical picture. People live with cavernous angioma all their lives and are not aware of its presence.
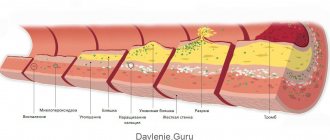
The structure of the neoplasm is predominantly dense, less often cavernous, characterized by the deposition of calcium salts in the walls, signs of thrombosis, the absence or small presence of elastic fibers and muscle tissue. Characterized by thinned, underdeveloped vascular walls. As a result of the absence of layers typical for normal vessels in the walls, they are characterized by high permeability.
Red blood cells penetrate through the walls into the surrounding medulla, which leads to the formation of characteristic pathologically altered brain tissue around the cavernoma, clearly visible during an MRI study. In general, the morphological heterogeneity of the structure of the neoplasm is revealed. May consist of lymphatic or blood vessels.
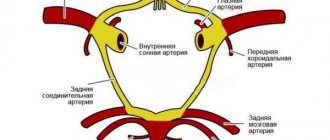
The first case is called lymphagioma, the second is called cavernous hemangioma, both develop in the brain and other parts of the body. A benign tumor consists predominantly of one cavity, less often - of several cavities. The internal space of the cavity is divided by partitions and filled with blood. Blood flow to the tumor occurs through small arterioles, and outflow through small venules.
Due to the small caliber of the feeding vessels, the blood pressure in the cavity of the cavernoma is small. Cavernous angiomas are not clearly visible when examined using selective CT and MRI, which makes diagnosis and detection at an early stage difficult. In 15% of cases, tumor-like compactions are located multiple times, more often – singly.
Diagnosis of cavernoma
This pathology is diagnosed using the following studies:
- CT;
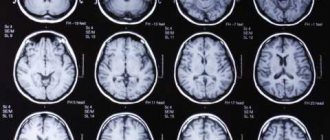
- MRI helps to determine the presence of cavities in the spinal and cerebral structures;
- EEG;
- functional magnetic resonance imaging;
- angiography – to examine blood vessels, identify their condition and detect pathology;
- detailed blood test - to detect the inflammatory process;
- examination of the cerebrospinal fluid to detect the presence of hemorrhage.
Do you want to know the cost of cancer treatment abroad?
* Having received data about the patient’s disease, the clinic representative will be able to calculate the exact price for treatment.
Types of disease
Pathology is classified according to histological structure and depending on location. The location of the tumor-like compaction determines the neurological symptoms. The most common are:
- Cavernous angiomas formed in the right temporal or left temporal lobe. Complications – hemianopsia (loss of visual fields), auditory hallucinations.
- Cerebellar cavernomas. They make up about 10% of all species. Complications of cerebellar angioma are a disorder of motor coordination and motor function in general.
- Cavernous angiomas arising in the left or right frontal lobe. Complications – mental disorders, loss of previously acquired practical skills, including labor, mental, and physical.
- Cavernous angiomas formed in the left or right parietal lobe. Complications – aphasia (speech impairment), problems with reading and performing simple arithmetic operations.
Tumor-like compaction in the area of the cerebral cortex is common and provokes epileptic seizures. In any localization, the development of the mental state of delirium is possible, which is accompanied by a disturbance of consciousness, a disorder of the functions of perception, attention, and thinking.
Forms
Angioma of the anterior hemisphere can be supplemented by damage in the normalization of mental functioning. The front parts of the brain regulate motivation and are able to imagine and carry out tasks. Their function is to manage their own actions and comprehend the result. The process of memory deterioration and uncontrollability of movements begins.
A cavernous tumor of the left frontal lobe causes consequences - alexia and a violation of the ordering of rhetoric. The person also lacks the desire to talk and take initiative.
Cavernous angioma of the right frontal lobe is the opposite of the previous one: the person is active in conversation. The patient is able to temporarily be in a state of passion, and sometimes emotional sensitivity increases. Most often, people show an optimistic attitude, because in most cases they do not suspect such an illness.
A cavernous neoplasm of the left temporal part occurs with a disorder of the speech and hearing apparatus. The patient has a poorly developed memory and almost no perception of other people's speech. In a dialogue, a person is able to use the same words repeatedly.
Hemangioma of the right temporal lobe is accompanied by symptoms: the inability to detect by ear the formation of a particular sound. In addition, a well-known voice may seem foreign to the patient.
Symptoms
Cavernomas formed in the brain are rarely accompanied by neurological symptoms. Neurological deficit (hemiparesis, impaired consciousness) usually occurs as a consequence of hemorrhages. The patient can live with a diagnosed benign tumor for a long time without experiencing discomfort. Signs of pathology:
- Epileptic and convulsive seizures.
- Focal hemorrhages in the subarachnoid space or in the cranial cavity, often recurrent.
- Occlusive hydrocephalus, which is characterized by impaired outflow of cerebrospinal fluid.
- Cerebral hypertension due to the accumulation of cerebrospinal fluid.
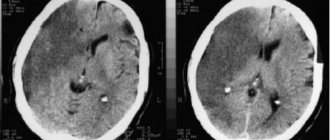
Due to the nonspecificity of the symptoms, difficulties arise in making the diagnosis of cavernous angioma. Focal tissue lesions that are observed on MRI or CT images are often mistakenly regarded as intracerebral tumors (gliomas). If the tumor is localized in the deep tissues of the brain, it is considered inoperable.
Main features
The main danger of cavernous angioma is that only 40% of patients have significant symptoms. If signs appear, they can be confused with many other neurological diseases. Only with an examination will it be possible to clearly say what exactly a person is suffering from. For this reason, you should not postpone a visit to the doctor if changes in your health have been noticed.
A brain cavernoma has the following symptoms:
- A person is often bothered by headaches, which gradually increase and are not treated with medications.
- Seizures of epilepsy may occur, during which the muscles contract convulsively.
- There is ringing and noise in the ears.
- The patient suffers from an inability to concentrate and has memory problems.
- There is numbness in the limbs, and complete paralysis may even occur.
- Speech impairment may be observed; the patient is unable to pronounce some letters, or is unable to construct entire sentences.
- The gait changes because the person suffers from poor coordination.
Cavernous angioma is most often discovered during a routine examination, or when another pathology is suspected. If a person does not go to doctors and does not experience negative symptoms, he may not know about the presence of a problem for the rest of his life . Given the fact that the disease is considered unpredictable, it is impossible to say for sure whether a person will live long or will have complications.
Reasons for education
The causes of the pathology have not been established. It is believed that congenital forms, which are more common, develop against the background of previous intrauterine infections, chronic and acute intoxications of the mother. The hereditary factor plays a role in the process of formation of neoplasms. Other possible reasons:
- Birth injuries to the fetus.
- Pregnancy over 40 years of age.
- Injuries in the head area.
- Inflammatory diseases of the brain.
The development of pathology can be influenced by factors: bad habits, a decrease in the body’s own immune defense, living in an unfavorable ecological zone.
Prevention
There is no way to prevent congenital vascular anomalies, as they are genetic disorders. To prevent acquired angiomas, you should lead a healthy lifestyle, eat right, avoid exposure to radiation and other harmful substances on the body, and monitor the condition of the cardiovascular system. It is necessary to engage in light physical activity, avoid stress and psycho-emotional stress.
I am engaged in the diagnosis and treatment of acne, I am fluent in the methods of therapeutic and hardware cosmetology to reduce the severity and eliminate age-related changes in the skin of the face and body. I have extensive theoretical knowledge and experience acquired during training and internships in leading cosmetology clinics in Europe.
Treatment
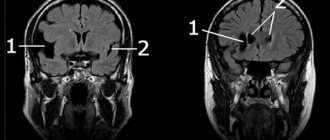
To make an accurate diagnosis, a comprehensive examination is carried out, which includes MRI, CT, angiography (less informative) and gamma topography. The MRI image clearly shows a rim around the tumor, consisting of hemosiderin, a pigment formed due to the breakdown of red blood cells.
CT images make it possible to differentiate cavernous angiomas from other types of tumors. In the first, there is no perifocal edema and stability of the midline brain structures is observed without signs of displacement. CT diagnostics is effective in the presence of foci of hemorrhage, which are clearly visible on the image for several days.
Treatment of cavernous angioma is selected individually depending on the size and location of the tumor in the brain. Asymptomatic pathology is subject to observation. Classic surgery in accessible localization is performed if neurological symptoms affecting the quality of life are observed.
Surgical intervention
Surgical resection of angioma is the priority treatment method. After surgery to remove a cavernoma from the brain area, negative consequences usually do not occur. During the operation, there are no difficulties in an easily accessible area due to the clearly defined border of the tumor.
In almost 50% of cases, a total ectomy can be performed. Tumor formations are easily separated from the brain matter. After surgery, neurological symptoms usually do not increase, which is due to the absence of nerve cells in the tumor structure.
Difficulties during surgery are often associated with the increased density of the tumor structure due to the large number of calcifications - areas with deposits of calcium salts. The risk of complications after surgery increases if the tumor is localized in the deep structures of the brain.
Radiosurgical method
Stereotactic radiosurgery is an alternative to conventional surgery. The procedure is indicated for the localization of cavernous cavities in hard-to-reach places and functionally important areas, for example, in the area of the brain stem. Under the influence of precisely directed ionizing radiation, neoplasm cells are destroyed, which leads to the formation of scar tissue and subsequent obliteration (overgrowth) of the cavity.
Radiosurgical treatment is aimed at preventing recurrent hemorrhages and epileptic seizures. According to statistics, after radiosurgical treatment the number of epileptic seizures is reduced in 73% of cases. Repeated hemorrhages in the next 2 years after the procedure are observed in 8-9% of cases, then the rate decreases to 3-4% of cases.
Cavernous malformations of the cerebellum
Removal of multiple cerebellar cavernomas
Cerebellar cavernomas account for 4–8% of all cavernomas and, as a rule, are localized in the cerebellar hemispheres. Cavernomas of the vermis and cerebellar peduncles are less common.
Clinical symptoms in cavernous malformations of the cerebellum, as in cavernomas of other locations, are caused by hemorrhages from the malformations. Acute or subacute development of the disease in the form of headache, nausea, vomiting in combination with brainstem-cerebellar symptoms is quite typical. General cerebral symptoms are especially characteristic of hemorrhages with blood spreading into the fourth ventricle or with the formation of large hematomas. Focal symptoms of cerebellar cavernomas are most often represented by dizziness, unsteadiness when walking, and loss of coordination in the limbs. Sometimes patients complain of double vision, but it can be quite vague, since, as a rule, it is associated not with damage to the oculomotor nerve system, but with vestibular disorders, which is manifested by the appearance of nystagmus. Symptoms that develop after hemorrhage from the cerebellar cavernoma can completely regress, but often persist for a long time.
Indications for removal of a cerebellar cavernoma should include hemorrhages manifested by severe cerebral and/or focal symptoms, especially repeated ones, as well as a progradient increase in focal symptoms. The formation of large hematomas causing occlusion of the cerebrospinal fluid pathways is an indication for urgent intervention. For large malformations with clinically compensated or subcompensated occlusion of the cerebrospinal fluid pathways, removal of the formation is also preferable.
You should refrain from surgery if the clinical picture is blurred, complete regression of symptoms after a single hemorrhage, especially in patients with cavernomas of the middle peduncle and medial parts of the cerebellar hemisphere, as well as in patients of an older age group and with a burdened somatic history.
The technique for removing cerebellar cavernomas does not have any significant differences from removing cavernomas of other locations. As with the removal of other space-occupying lesions of the cerebellum, performed with the patient in a sitting position, special attention should be paid to the prevention of air embolism. The risk of developing cerebral edema and rapidly developing occlusion of the cerebrospinal fluid pathways, which may be caused by impaired venous outflow, should also be taken into account. In the postoperative period, if necessary, external ventricular drainage should be installed. With cavernomas of a paratrunk location, there is a risk of damage to the vessels supplying the trunk with the development of corresponding complications.
Forecast
The prognosis is mostly favorable. The exception is when a cavernoma is localized deep in the brain tissue or in the brainstem area, when surgical intervention is required due to the high risk of sudden life-threatening hemorrhages.
Cavernous angioma is a benign tumor consisting of abnormal elements of the circulatory system. When small in size and without hemorrhages, it does not pose a threat to life. Often, patients with diagnosed cavernoma live for many years without experiencing discomfort due to the diagnosis.
610
What is this
It has already been said that cavernous angioma of the brain is a vascular neoplasm that is benign in nature. The pathology includes lymphatic or blood vessels. In children, pathology is more often diagnosed, because during fetal development their capillaries, veins and arteries can become intertwined.
The size of neoplasms can average from a millimeter to several centimeters or more. Large areas are rarely affected. The pathology consists of cavities, their surface is strewn with endothelial cells, and there is plasma inside. Often the pathology does not have clear symptoms, which makes it difficult to identify.
If a person notices signs of a brain cavernoma, then it is important to see a doctor immediately. Only a specialist will be able to make a diagnosis and decide what treatment to prescribe in a particular case. Inaction or improper therapy can lead to complications.
General ideas about cavernomas and their causes
The central nervous system can be a substrate for the emergence of a large number of different tumors: gliomas, astrocytomas, medulloblastomas. But in addition to neoplastic formations developing from cells of nervous tissue, the brain can be affected by a tumor of vascular origin, because the vascular bed supplies blood to all organs of the human body.
Hemangioma is a neoplasm of endothelial cells. It is usually associated with the general blood flow. Outwardly it looks like an expanded vascular formation, an aneurysm. Cavernous angioma (or cavernoma) is a type of vascular formation that consists of several vascular cavities with thin walls. As a rule, these chambers have different sizes, sizes and volumes. But their main characteristic is that they are clearly demarcated from the brain parenchyma surrounding them.
Cavernous hemangioma is a tumor that does not have a clear organic and functional connection with the general blood flow. However, next to it there is usually an artery or vein, usually also deformed like an aneurysm. It is this that is the source of blood supply. Therefore, angiomas fill with blood and can, under certain conditions, cause hemorrhage.
Among the causes, neurologists and oncologists prefer to recognize a genetically determined defect. The genes responsible for the pathology have already been discovered. The inflammatory theory also remains relevant today.
Origin of cavernous angioma
Cavernous hemangioma is a type of infantile hemangioma. It occurs in the vast majority of cases in children and is congenital, but not hereditary. It is a pathological proliferation of blood vessels that form cavities (cavities) filled with blood. Under a microscope, overgrown vessels are visible, chaotically woven into knots.
The disease is benign in nature, although it grows rapidly and grows into surrounding tissues. It is rare - it accounts for 7% of vascular tumors according to WHO observations. The ICD-10 code is D18.0.
The exact causes of the disease are unknown. It is assumed that in the first trimester of pregnancy there is a disruption in the formation of the fetal vascular system. Predisposing factors: prematurity, pregnancy pathology, multiple pregnancies, viral diseases, bad habits and other factors that negatively affect the condition of the unborn child.
This type of tumor also occurs in adults, but is extremely rare. Reasons: disruption of blood vessels due to diseases of internal organs, toxic effects of certain drugs, radiation, excessive exposure to UV rays, poor ecology.
Liver hemangioma is a mysterious disease; the reasons for the development and growth of tumors have not yet been precisely established. Cavernous hemangioma occurs in approximately 2% of the population, with men affected less frequently than women. The disease can occur at absolutely any age; as a rule, it is diagnosed in patients 30-50 years old.
The disease is characterized by the proliferation of vascular walls with the formation of cavities (cavities). In fact, hemangioma is a benign formation, but it necessarily requires observation and, if necessary, timely and high-quality treatment.
Cavernous hemangioma does not pose a threat to life; if it is formed near physiological openings and on the mucous membranes, it can cause a lot of discomfort. When a hemangioma grows near the external auditory canal or eyes, there is a risk of deafness and blindness.
Cavernous hemangioma is a benign tumor in the liver. Symptoms are absent in most patients, often becoming obvious only when the tumor increases significantly. The incidence of the disease is approximately 7% of the population. More often, the pathological process is found in women.
The liver is an organ that lacks nerve endings.
What then worries people who, when they come to see a doctor, complain of pain under the ribs on the right side? Often one of the causes of pain in the right hypochondrium is cavernous hemangioma of the liver, which poses a serious threat not only to the organ, but also to health in general. Everything about the causes, symptoms and features of therapy is in this material.
There are two types of this disease: hereditary or sporadic.
- The mechanism of the congenital type of the disease is considered to be more studied, but there is also evidence of an autosomal dominant nature of inheritance; characteristic genes of the seventh chromosome have been identified and established, which affect the formation of pathological vascular ligaments
- The causes of sporadic tumors are still unknown. There are three scientific theories: the result of radiation, inflammation of the immune system, infection.
Localization of angiomas:
- 80% of angiomas are located in the upper lobes of the central brain. 65% of their component falls on the frontal, temporal and posterior parts. 15% on vascular occurrences of optical convexity.
- 8% are neocerebellum hemangioma.
- 2.5% vascular configurations in the dorsal medulla.
Detection is determined by the location of the tumor. The first signs are: migraine, not eliminated by medications; convulsions; sounds in the ears; disorganization of coordination; bouts of vomiting and nausea; weakness of the limbs; degradation of hearing and vision; memory distortion; disorder in speech. It happens that the angioma is “silent”. People don't even know about the disease. The tumor is detected when tested for other diseases or when it manifests itself in other family members.
Treatment of cavernoma should begin with a comprehensive diagnosis according to a regimen prescribed by doctors, which is created personally for the patient.
The unified diagnostic system includes types of research: detailed bioanalyses of blood (for the presence of anemia), spinal emulsion (for the presence of hemorrhages).
Recognition using tools:
- The angiography method is an X-ray examination of capillaries using a contrast solution. The image taken will make it possible to determine the level of compression or decomposition of the brain vessels, based on the reformation in the capillary septum and the location of problem areas. This recognition structure is aimed at identifying a perfusion defect in the brain. Clear determination of the location, quantity and patterns of angioma, as well as detection of impaired vessel integrity. To carry out this diagnostic, a specially equipped office is required. First, local anesthesia is performed, and then a flexible tube is inserted into the vessel, moving it towards the infected part. The contrast composition, placed in the circulatory structure, is quickly placed along the vascular network, then a couple of images are taken, based on which an accurate conclusion is drawn.
- The tomography method does not cause any inconvenience, the procedure is informative. It is allowed to carry out with or without the use of a contrast composition. As a result, the most accurate layer-by-layer X-ray images obtained allow a more accurate study and examination of the pathology. The operation takes place in specialized rooms using the necessary tomography equipment.
- The magnetic resonance imaging (MRI) technique is relatively affected by the previous method. MRI images are detailed and three-dimensional. The process provides even more information about the disease, but the procedure is considered quite expensive.
- The electroencephalography method helps to study the biological capabilities of the brain center, identify the location of the angioma, its size. When a tumor is present, the doctor distinguishes between differences in the signal sent by brain processes.
- Radiotherapy – cavernous angioma of the brain is curable with this technique. It is a very long process, capable of containing about 30-40 procedures. Radiochemistry is the opposite. To destroy a tumor, only one procedure is enough - a gamma knife. Strong radiation can lead to DNA erosion of pathogenic cells. After gamma phonation in the septa, the blood capillary can be damaged, as well as the internal layers of the blood vessel.
Immediate treatment is the safest way to get rid of cavernoma. There is no universal drug that can cure a tumor. The prescription of a course of therapy is determined by the fact that cavernous angioma does not bring discomfort to most patients, and lasting disability is noticed in most cases with recurrent hamatocoelia from deeply located angiomas or from tumors of the brain stem - parts that are difficult to access for surgical change.
Even a benign course of the disease cannot promise the absence of problems in the future, and a prompt operation can eliminate the danger of negative consequences.
Experts advise immediate treatment in cases of cavernous angioma of the skin, manifested by extravasation, or convulsive syndromes. Treatment is required for malformations located in the energetic parts of the brain and caused by hematomyelia, a neurological approach and an epileptic attack with dangerous sizes of angioma.
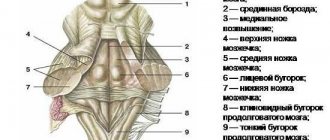
Cavernous malformations and brainstem hematomas
Brainstem cavernomas occupy a special place among central nervous system cavernomas, on the one hand, due to the danger of the disease itself, and on the other, due to the complexity of operations on the brainstem. In the brainstem, cavernomas are most often located at the level of the pons. The second most common is the midbrain. Least often, brainstem cavernomas can be identified in the medulla oblongata. Like cavernomas of other localizations, trunk cavernomas, especially large ones, can spread to neighboring formations - the thalamus optic, the middle cerebellar peduncle. Very rare observations include cavernomas of craniospinal localization.
In most cases, even with small-volume hemorrhages, distinct focal symptoms are detected. This is due to the very close arrangement of conductors and nuclei in the brain stem. Focal neurological symptoms during hemorrhage, with extremely rare exceptions, develop against the background of preserved consciousness; in half of the patients, against the background of headache. The structure of the focal syndrome most often includes signs of damage to both the nuclei of the cranial nerve and the pathways. Pontine lesion syndromes prevail due to the most common localization of malformations in this part of the brain stem. It should be noted that the classic brain stem lesion syndromes described in cerebrovascular accidents are not typical for patients with this form of pathology.
The severity of the patient's condition is largely determined by symptoms such as dizziness, impaired movements of the eyeballs, peripheral paresis of the facial nerve, bulbar or pseudobulbar disorders, paresis of the limbs and trunk ataxia. In addition to focal symptoms, hypertensive symptoms may develop due to occlusion of the cerebrospinal fluid pathways, especially with midbrain cavernomas.
In a small proportion of patients with cavernous malformations, there is no obvious clinical hemorrhage, or it can be traced only at the onset of the disease. The undulating course of the disease in the form of repeated episodes of the appearance and subsequent partial regression of symptoms of brain stem damage over many years is often regarded as circulatory failure in the vertebrobasilar system or a demyelinating process. Gradually worsening neurological symptoms in these cases are most likely due to changes occurring in the cavernous malformation - thrombosis of its cavities, impaired venous outflow and increase in size.
With malformations of the midbrain in the area of the roof and/or tegmentum, symptoms of partial damage to the third nerve or Parinaud's syndrome most often occur, which are combined with signs of damage to the medial lemniscus in the form of sensory disturbances contralateral to the lesion (mainly superficial), or contralateral tremor is noted (due to damage to the red nucleus or fibers of the superior cerebellar peduncle in the area from Wernecking's decussation to the red nucleus). Isolated damage to the third nerve is extremely rare.
When the malformation is localized exclusively in the cerebral peduncle, pyramidal symptoms contralateral to the lesion and truncal ataxia, caused by damage to the corticopontine tracts, dominate.
When the malformation is localized in the area of the pons, the structure of the neurological syndrome is largely determined by the topography within the pons, namely: damage to the base, tegmentum, or both of these parts of the pons; location relative to the midline and long pons (caudal, rostral). It is extremely rare to observe isolated damage to either the CN nuclei or long conductors. As a rule, their defeat is combined. When the tegmentum of the bridge is damaged, disturbances in the horizontal movements of the eyeballs prevail, either due to damage to the fibers of the medial longitudinal fasciculus and the “center” of horizontal gaze, or only due to the nucleus of the VI nerve. The close anatomical and functional connection between the horizontal gaze regulation system and the vestibular nuclei explains the frequent combination of disturbances in the horizontal movements of the eyeballs with systemic dizziness, nausea and vomiting. Disturbances in the horizontal movement of the eyeballs are often combined with dysfunction of the facial muscles (damage to the nucleus or root of the VII nerve), as well as contralateral disorders of superficial and deep sensitivity (damage to the spinothalamic tract and medial lemniscus). Signs of an isolated lesion of the VII nerve are observed extremely rarely, as an exception; more often they are combined with symptoms of damage to either the VI nerve or the fibers of the medial longitudinal fasciculus and the “center” of horizontal gaze. When the base of the bridge is affected, pyramidal symptoms dominate, and with total damage to the bridge, severe symptoms are revealed, both from the base of the bridge and the tire.
When the medulla oblongata is affected, the clinical picture is dominated by a pronounced bulbar syndrome, most often combined with signs of damage to the medial lemniscus in the form of impaired superficial sensitivity and moderately severe trunk ataxia.
The clinical well-being of the patient is the leading indicator that justifies the refusal of surgical treatment and the choice of conservative management in patients with small hematomas, even in cases of acute and subacute hemorrhages. In these situations, much depends on the decision of the patient himself, who is informed about the possible complications of the operation, and about the possible further course of the disease if the operation is refused. When selecting patients for surgical treatment, one should take into account the severity of the patient’s condition at the time of surgery, the volume of hemorrhage (hematoma), the number of previous hemorrhages, the localization of the malformation and its proximity to the surface of the brain stem.
There are significant differences in the outcome of surgical treatment in the main groups - hematomas without MR signs of malformation and with cavernous malformations. In cases of hematomas, the first month from the moment of hemorrhage is a subacute hematoma, suggesting the most favorable outcome of surgical intervention. Delaying surgery leads to the formation of a chronic hematoma, the development of scar changes, and a decrease in the volume of the hematoma, which creates additional difficulties during its removal and affects the outcome of the operation. We believe that in patients with recurrent hemorrhages, it is advisable to perform surgery during the period of persistent hematoma. In case of resorption of hemorrhage, one should refrain from surgery and perform it only if the next one develops, without wasting time.
The choice of surgical approach is based on a thorough study of the topography of the formation according to MRI data. Removal of the hematoma and/or malformation is performed from the side closest to the surface of the brain stem.
Removal of chronic hematoma of the cerebral pons from suboccipital craniotomy with access through the fourth ventricle
Most often, median suboccipital craniotomy with access through the fourth ventricle is used. This is due to the fact that most of the hematomas and cavernous malformations are located subependymal, in the area of the tegmentum of the pons. When the pathological formation is located ventrolaterally, a retrosigmoid suboccipital approach is often used, which, however, does not allow a sufficiently complete inspection of the hematoma cavity in all cases or a good exposure of the cavernous malformation. In such cases, the use of retrolabyrinthine presigmoid or subtemporal approaches is justified, since they provide a wider viewing angle of the surgical field and, accordingly, a greater possibility of radical removal of the malformation and chronic hematoma capsule. In recent years, there have been separate reports on the possibility of using, with a ventral location of the formation at the level of the bridge, transsphenoidal access and removal of cavernoma using an endoscope, as well as transoral transclival access. When removing a hematoma and/or midbrain cavernoma, a subtentorial-supracerebellar or occipital interhemispheric approach with dissection of the tentorium cerebellum is used. Subchoroidal access can also be used. In some cases, for example, when removing a malformation in the anterior parts of the cerebral peduncle, a pterional approach can be used.
Today, most brainstem surgeries are performed with mandatory intraoperative neurophysiological monitoring, which significantly reduces the risk of damage to the most important structures of the brainstem during surgery. The two main methods most commonly used are rhomboid fossa mapping and “motor evoked potential” recordings.
After a thorough examination of the fundus, it is often possible to detect the area where the formation is closest to the ependyma, which can be sharply thinned, and to approach the CM or to open the hematoma cavity, it is enough just to separate the brain with the thin jaws of anatomical tweezers. With a deeper location of the vascular malformation, it is necessary to dissect the medulla in a small area. Dissection of the bottom of the fourth ventricle along the midline between the nuclei of the facial nerves is considered relatively safe. When the malformation is localized below the stria medullaris, dissection of the bottom of the fourth ventricle is recommended in the area of the median posterior fissure caudal to the obex or along the intramedullary and lateral grooves.
When removing cavities and hematomas of the trunk, narrow spatulas are used only to separate the cerebellar tonsils. Providing access to the vascular malformation itself is carried out with instruments manipulated by the surgeon: thin suction, tweezers with narrow jaws, microscissors, etc. Since there is practically no blood flow in cavernomas, they can and should be removed by biting, which reduces the traumatic nature of the operation.
For encapsulated hematomas, after removing their contents - blood clots of varying degrees of lysis and organization - it is advisable to mobilize the capsule, cutting it into fragments, and remove it, if possible, completely.
An increase in symptoms (damage to the cranial nerve or conductors) immediately after surgery is noted, according to various sources, in 29% - 67% of cases, however, in approximately half of the patients, these symptoms subsequently partially or completely regress, which suggests a persistent neurological defect in approximately 15% - 30% of those operated on. Improvement in the condition of patients immediately after surgery is most often observed after removal of hematomas. When removing cavernous malformations outside the hemorrhage stage, the outcome in most cases is unsatisfactory: symptoms increase in 73% of patients.